Cannabidiol mitigates alcohol dependence and withdrawal with neuroprotective effects in the basolateral amygdala and striatum – Nature
Report on the Therapeutic Potential of Cannabidiol for Alcohol Use Disorder in Alignment with Sustainable Development Goal 3
Executive Summary
This report details a preclinical investigation into the efficacy of Cannabidiol (CBD) as a treatment for Alcohol Use Disorder (AUD). The study’s objectives are directly aligned with the United Nations’ Sustainable Development Goal 3 (Good Health and Well-being), particularly Target 3.5, which aims to “strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.” By exploring novel pharmacotherapies, this research seeks to provide evidence-based solutions to a pervasive public health issue that impedes global progress toward health and well-being for all. The findings indicate that chronic CBD administration significantly mitigates behavioral and neurobiological aspects of alcohol dependence, positioning it as a promising candidate to help achieve the objectives of SDG 3.
1.0 Introduction: Addressing Alcohol Use Disorder as a Global Health Priority
Alcohol Use Disorder (AUD) represents a significant global health challenge, imposing substantial social, economic, and health burdens that directly contravene the principles of Sustainable Development Goal 3 (Good Health and Well-being). The limited efficacy of current treatments underscores the urgent need for innovative therapeutic strategies to meet SDG Target 3.5. Cannabidiol (CBD), a non-psychotropic compound, has emerged as a promising candidate due to its favorable safety profile and diverse pharmacological properties, including neuroprotective, anxiolytic, and anti-inflammatory effects. This study evaluates the therapeutic potential of chronic CBD administration in validated rodent models of alcohol dependence, aiming to provide critical preclinical evidence to support its development as a tool for combating AUD and advancing global health objectives.
2.0 Methodology
The study utilized two complementary and validated rodent models to investigate the effects of chronic CBD administration on multiple facets of alcohol dependence. All procedures were conducted in compliance with institutional and national guidelines for animal care.
2.1 Chronic Intermittent Ethanol (CIE) Exposure Model
This model was used to assess CBD’s effects on established alcohol dependence and withdrawal.
- Subjects: Adult Wistar rats (male and female).
- Procedure: Rats were trained to self-administer alcohol and then exposed to chronic intermittent ethanol vapor to induce dependence.
- Treatment: Following dependence induction, rats received daily subcutaneous injections of CBD (30 mg/kg or 60 mg/kg) or a vehicle.
- Assessments:
- Alcohol self-administration and motivation (Progressive Ratio test).
- Somatic and behavioral signs of withdrawal (locomotor activity, anxiety, mechanical sensitivity).
- Stress-induced reinstatement of alcohol-seeking behavior.
- Alcohol metabolism.
- Neuronal excitability in the basolateral amygdala (BLA) via electrophysiological recordings.
2.2 Ethanol Vapor Self-Administration (EVSA) Model
This model was employed to evaluate CBD’s impact on the volitional aspects of alcohol consumption and the development of dependence.
- Subjects: Adult Wistar rats (male and female).
- Procedure: Rats voluntarily self-administered ethanol vapor over an extended period, modeling the escalation of intake.
- Treatment: Rats received daily CBD (60 mg/kg) or vehicle injections prior to test sessions.
- Assessments:
- Voluntary alcohol vapor intake.
- Saccharin self-administration (control for general reward-seeking behavior).
- Neurodegeneration markers (Caspase-3, NeuN, GFAP, NG2) in key striatal subregions via immunohistochemistry.
3.0 Key Findings: CBD Mitigates Alcohol Dependence and Neurodegeneration
The results provide compelling evidence for CBD’s therapeutic effects on AUD, supporting its potential to contribute to the achievement of SDG Target 3.5.
3.1 Effects on Alcohol Dependence and Withdrawal (CIE Model)
- Reduced Alcohol Intake: Chronic CBD administration (60 mg/kg) significantly reduced alcohol self-administration and motivation for alcohol during withdrawal without affecting alcohol metabolism or general locomotor activity.
- Alleviated Withdrawal Symptoms: CBD decreased somatic withdrawal signs, withdrawal-induced anxiety, and mechanical hypersensitivity.
- Prevented Relapse: CBD attenuated both alcohol-seeking behavior during extinction and stress-induced reinstatement, a critical factor in preventing relapse and supporting long-term recovery.
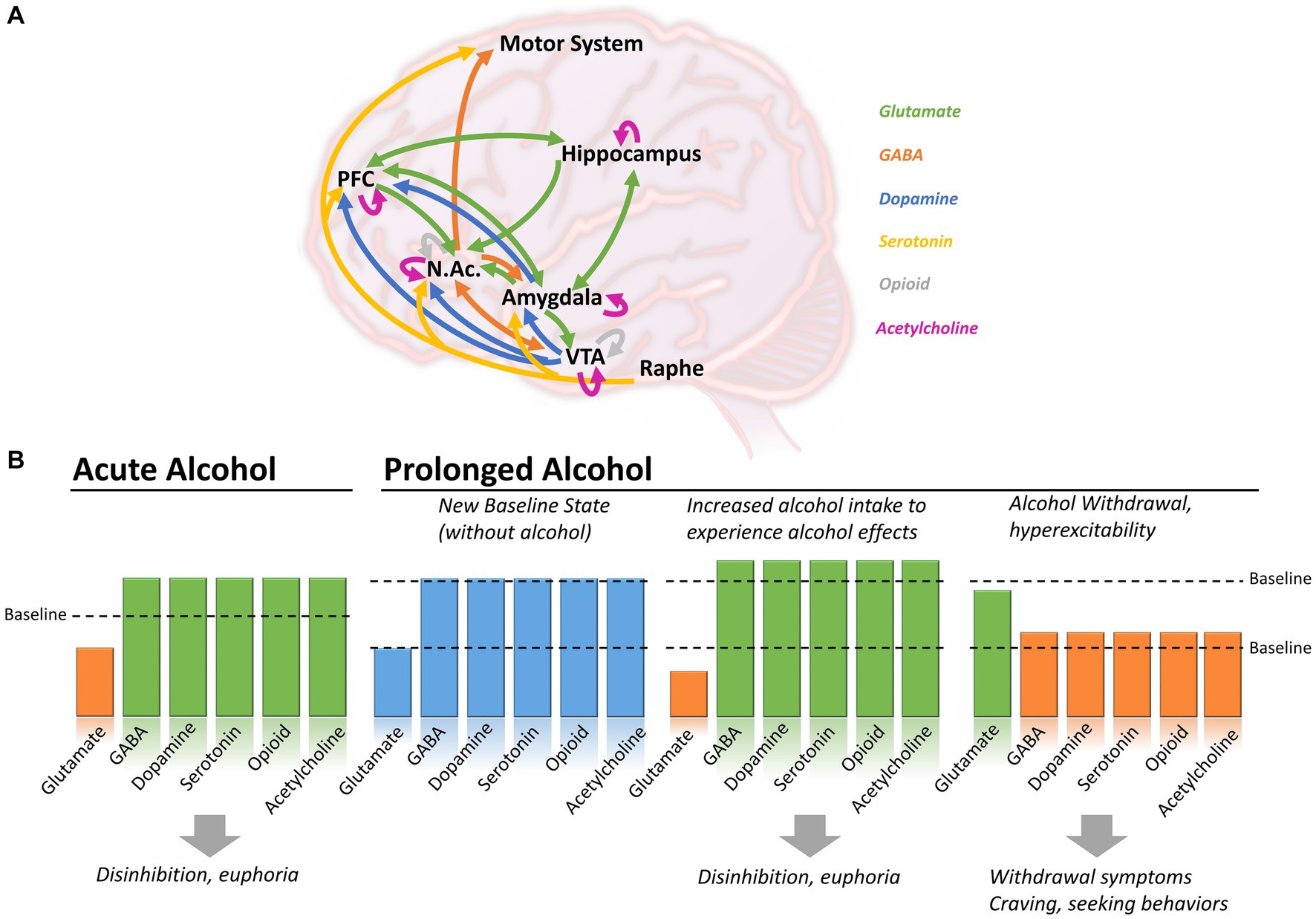
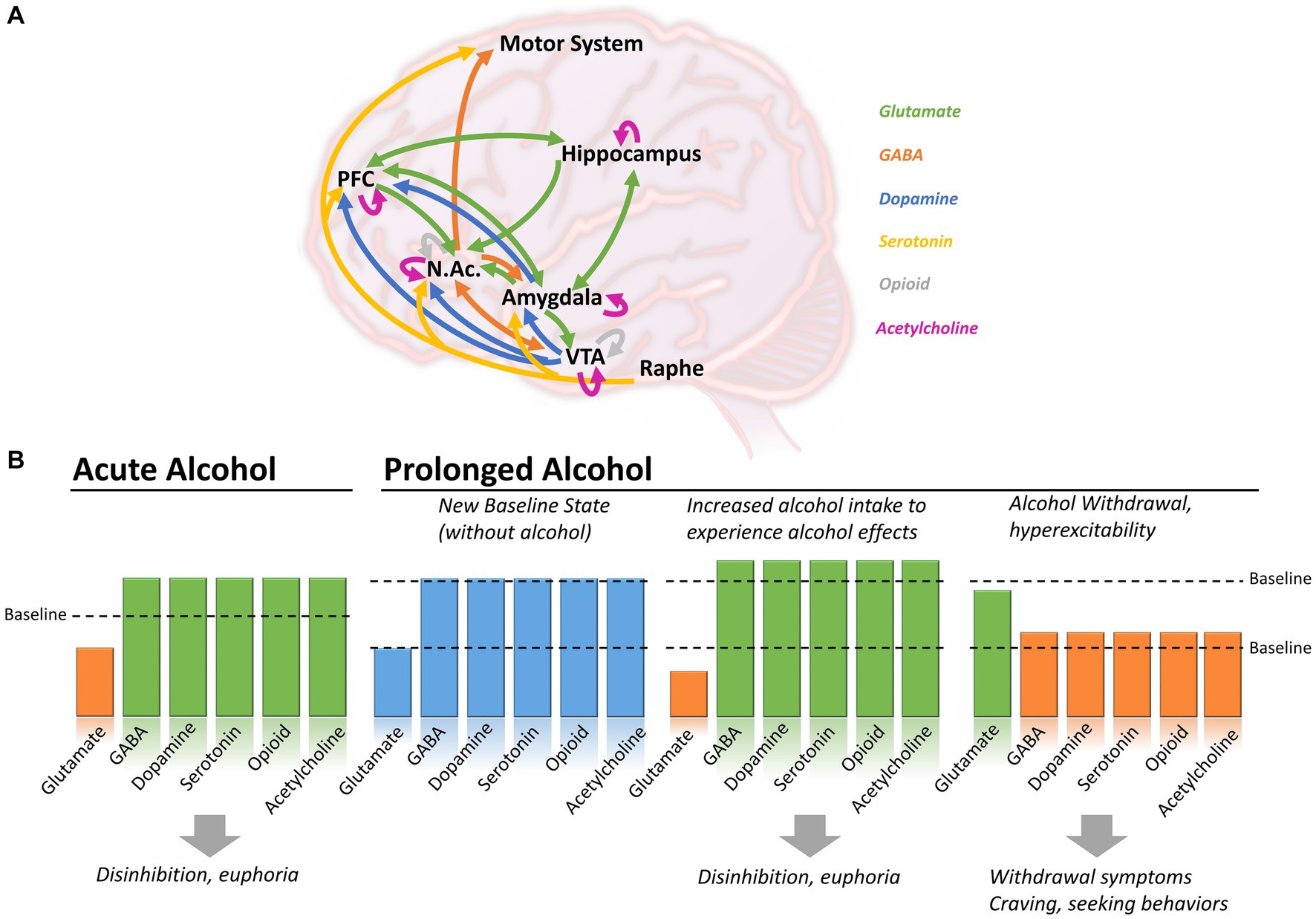
- Normalized Neural Function: Electrophysiological recordings revealed that CBD reversed alcohol-induced decreases in neuronal excitability in the basolateral amygdala, suggesting a key mechanism for its therapeutic action.
3.2 Effects on Voluntary Alcohol Intake and Neuroprotection (EVSA Model)
- Reduced Voluntary Consumption: CBD specifically reduced voluntary alcohol intake during the escalation phase of the EVSA model, an effect not observed in saccharin self-administration, indicating specificity for alcohol-related behaviors.
- Prevented Neurodegeneration: Immunohistochemical analysis showed that CBD prevented alcohol-induced neurodegeneration in the nucleus accumbens shell and dorsomedial striatum—brain regions critical for the volitional control of behavior. This neuroprotective effect is a vital component for restoring brain health, a cornerstone of SDG 3.
4.0 Discussion and Conclusion: Advancing SDG 3 Through Novel AUD Treatment
This study demonstrates that chronic CBD administration effectively mitigates the behavioral and neurobiological consequences of alcohol dependence in robust preclinical models. The findings have significant implications for public health and the pursuit of Sustainable Development Goal 3 (Good Health and Well-being).
By reducing compulsive alcohol intake, alleviating debilitating withdrawal symptoms, and preventing stress-induced relapse, CBD addresses the core challenges of AUD treatment. These actions are fundamental to achieving SDG Target 3.5. The mechanisms underlying these benefits—namely, the normalization of neuronal excitability in the BLA and the prevention of neurodegeneration in the striatum—highlight CBD’s potential to restore brain circuits disrupted by chronic alcohol use. Preserving the functional integrity of neural systems involved in emotional regulation and reward processing is crucial for sustainable recovery and improved mental health.
In conclusion, this report provides strong preclinical support for CBD as a viable pharmacotherapy for AUD. Its multifaceted effects on both behavior and neurobiology offer a comprehensive approach to treatment. Further clinical investigation is warranted to translate these findings into effective therapies for human populations, thereby providing a powerful new tool to combat substance abuse and advance the global agenda for good health and well-being for all.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
The primary Sustainable Development Goal (SDG) addressed in the article is:
-
SDG 3: Good Health and Well-being
Explanation: The article directly addresses a major public health concern, stating that “Alcohol use disorder (AUD) remains a pervasive public health issue with limited effective treatments.” The entire study is dedicated to investigating a novel therapeutic approach (Cannabidiol, or CBD) to treat this disorder, which aligns perfectly with SDG 3’s mission to “ensure healthy lives and promote well-being for all at all ages.” The research aims to find more effective pharmacotherapies to mitigate the “significant health, social, and economic burdens posed by AUD.”
2. What specific targets under those SDGs can be identified based on the article’s content?
Based on the article’s focus, the following specific targets under SDG 3 are identified:
-
Target 3.5: Strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.
Explanation: This target is central to the article. The research is an explicit attempt to strengthen the treatment of the “harmful use of alcohol.” The study investigates how chronic CBD administration can “reduce alcohol self-administration,” “decrease motivation for alcohol,” and “attenuate alcohol-seeking behavior and stress-induced reinstatement.” These are all core components of treating substance abuse and dependence. The introduction highlights that “less than 10% of individuals with AUD receive approved medications,” underscoring the “urgent need for novel therapeutic approaches,” which this study aims to provide. -
Target 3.4: By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
Explanation: Alcohol Use Disorder is a non-communicable disease and a significant mental health condition. The article connects to this target in several ways:- Treatment of a Non-Communicable Disease: The study explores a treatment that could reduce the severe health consequences of AUD, including the “alcohol-induced neurodegeneration” which contributes to long-term morbidity.
- Promotion of Mental Health and Well-being: The article notes that AUD is characterized by a “negative emotional state during withdrawal” and that CBD has “anxiolytic” properties. The results show that CBD “attenuated withdrawal-induced anxiety-like behaviors,” directly addressing the mental health component of the disorder.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
Yes, the article provides several specific preclinical indicators used to measure the effects of CBD on AUD, which serve as proxies for measuring progress towards the identified targets.
-
Behavioral Indicators of Treatment Efficacy (Target 3.5):
- Reduction in Alcohol Consumption: The study measures “alcohol self-administration” and “voluntary alcohol intake” in rodent models. The finding that “CBD reduced voluntary alcohol intake during the escalation phase” serves as a direct indicator of reduced harmful alcohol use.
- Reduction in Motivation and Craving: Progress was measured using a “progressive ratio (PR) schedule,” where the result that “CBD… lowered the progressive ratio breakpoint for alcohol self-administration” indicates reduced motivation for alcohol.
- Alleviation of Withdrawal Symptoms: The study uses a “somatic withdrawal signs” scale and an “elevated plus maze” to assess withdrawal. The findings that CBD “reduced overall somatic withdrawal severity” and “attenuated withdrawal-induced anxiety-like behavior” are key indicators of effective treatment.
- Prevention of Relapse: The study measures “stress-induced reinstatement” of alcohol seeking. The conclusion that “CBD blocked stress-induced reinstatement of alcohol seeking” is a critical indicator for preventing relapse, a primary goal of substance abuse treatment.
-
Neurobiological Indicators of Health Improvement (Target 3.4 & 3.5):
- Prevention of Neurodegeneration: The article uses “immunohistochemical analyses” to measure markers of cell death (Cleaved Caspase-3) and neuronal health (NeuN, GFAP, NG2). The finding that “CBD prevented alcohol-induced neurodegeneration in the nucleus accumbens shell and dorsomedial striatum” is a biological indicator of preventing the physical damage caused by AUD.
- Normalization of Brain Function: “Electrophysiological recordings” were used to assess neuronal health. The result that “CBD reversed alcohol-induced decreases in neuronal excitability in the basolateral amygdala” serves as an indicator of restoring normal brain function, which is crucial for promoting mental well-being and treating the underlying pathology of the disease.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators Identified in the Article |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.5: Strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol. |
|
| SDG 3: Good Health and Well-being | 3.4: Reduce premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being. |
|
Source: nature.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0


























;Resize=805#)