Assessment of nutritional status and eating behaviours in patients with chronic inflammatory bowel disease: a pilot study – Nature
Report on Nutritional Status and Eating Behaviours in Patients with Inflammatory Bowel Disease (IBD)
Introduction and Alignment with Sustainable Development Goals (SDGs)
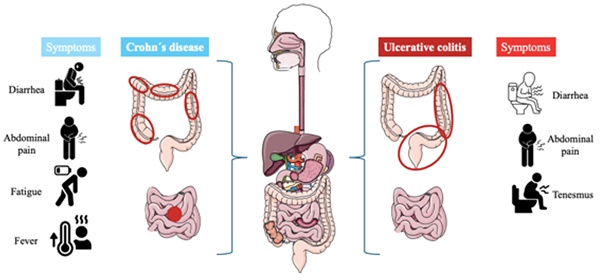
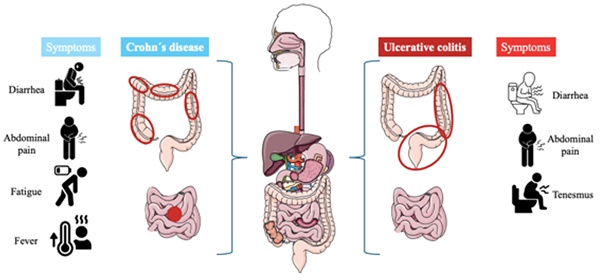
Inflammatory Bowel Diseases (IBD), including Ulcerative Colitis (UC) and Crohn’s Disease (CD), present a significant challenge to global health, directly impacting Sustainable Development Goal 3 (Good Health and Well-being). The absence of standardized dietary recommendations for IBD patients complicates disease management and can compromise nutritional status, working against Sustainable Development Goal 2 (Zero Hunger), which aims to end all forms of malnutrition. This report details a study that evaluates the dietary habits of IBD patients to inform strategies that enhance health outcomes and quality of life, thereby supporting the achievement of these critical SDGs.
Methodology
A study was conducted at the IRCCS Ca’ Granda Foundation Ospedale Maggiore Policlinico of Milan between April 2020 and July 2022. The objective was to assess the dietary patterns of patients with UC and CD, with a specific focus on identifying commonly preferred and avoided foods.
Key Findings and Analysis
Nutritional Status and Disease Activity
The investigation revealed that a majority of participants were in clinical remission and maintained a normal nutritional status. This finding is crucial for SDG 3, as it indicates that with proper management, individuals with chronic non-communicable diseases can maintain a state of well-being.
- UC Patients: 67.4% were in remission according to the Mayo score.
- CD Patients: 80.9% were in remission based on the Harvey-Bradshaw Index (HBI).
- CD patients exhibited a higher weight compared to both UC patients and the control group.
Prevalence of Restrictive Diets: A Challenge to SDG 2
A significant number of patients adopted restrictive diets, which, while intended to manage symptoms, pose a risk to adequate nutrient intake and could lead to malnutrition, undermining the objectives of SDG 2 (Zero Hunger). The lack of professional supervision for these dietary changes highlights a gap in patient care.
- Lactose-Free Diets: This was the most common restriction.
- UC Patients: 21.3%
- CD Patients: 17.4%
- Controls: 11.6%
- Gluten-Free Diets: Also prevalent, particularly among UC patients.
- UC Patients: 23.4%
- CD Patients: 13.4%
- Controls: 9.3%
- Low-FODMAPS Diet: Adoption was minimal among all groups.
Notably, no statistically significant associations were found between these dietary patterns and disease activity, suggesting that unsupervised restrictions may not provide clinical benefits and could unnecessarily compromise nutritional health and quality of life.
Fibre Avoidance and Its Impact on Intestinal Health
A critical finding was the widespread avoidance of dietary fibre among IBD patients, a practice that can negatively affect intestinal homeostasis and long-term health, a key concern for SDG 3.
- CD Patients: 52% avoided fibre.
- UC Patients: 45% avoided fibre.
- Controls: Only 5% avoided fibre.
This avoidance is counterproductive, as fibre is essential for maintaining a healthy gut microbiota. The alteration of microbiota composition due to low fibre intake can exacerbate intestinal health issues, creating a cycle of poor health outcomes.
Conclusions and Recommendations for Sustainable Health Management
The study concludes that IBD patients frequently implement dietary restrictions, primarily lactose-free and gluten-free diets, which impact their quality of life and nutritional intake without a clear link to disease activity. The prevalent avoidance of fibre is a significant concern that requires intervention.
To align with the principles of SDG 3 (Good Health and Well-being) and SDG 2 (Zero Hunger), the following recommendation is proposed:
- Healthcare providers should actively encourage the supervised intake of dietary fibre in IBD patients. This approach aims to prevent detrimental alterations to the gut microbiota, promote intestinal homeostasis, and ensure nutritional adequacy, contributing to a sustainable and holistic model of care for individuals with chronic inflammatory conditions.
Analysis of Sustainable Development Goals (SDGs) in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 2: Zero Hunger
- The article directly addresses nutrition by evaluating the diets of patients with Ulcerative Colitis (UC) and Crohn’s Disease (CD). It discusses “normal nutritional status,” “dietary restrictions affecting nutrient intake,” and the avoidance of specific food groups like fibre. This connects to SDG 2’s broader aim of ending all forms of malnutrition and ensuring proper nutrition.
-
SDG 3: Good Health and Well-being
- The core subject of the article is the management of non-communicable inflammatory bowel diseases (IBD). It examines how diet impacts disease activity and “quality of life.” The study’s aim to find better dietary recommendations to manage these chronic conditions and improve patient well-being aligns directly with SDG 3.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Target 2.2: End all forms of malnutrition
- The article’s focus on the “normal nutritional status” of the study population and the concern that “prevalent dietary restrictions affecting nutrient intake” could lead to nutritional imbalances relates to this target. It highlights the challenge of maintaining proper nutrition in a specific population group (IBD patients), which is a key aspect of ending malnutrition in all its forms.
-
Target 3.4: Reduce by one-third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being
- The study investigates dietary management as a tool for treating IBD, which are non-communicable diseases. It explicitly mentions that dietary restrictions affect the “quality of life” of patients and measures “disease activity.” This directly corresponds to the goal of improving treatment and promoting well-being for individuals with chronic health conditions.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Indicators for Target 2.2 (End all forms of malnutrition)
- Nutritional Status: The article explicitly states that the study evaluated patients for “normal nutritional status,” which serves as a direct indicator of malnutrition.
- Prevalence of Dietary Restrictions: The study measures the percentage of patients on specific diets, such as “Lactose-free diets (21.3% UC, 17.4% CD)” and “gluten-free diets (23.4% UC, 13.4% CD).” This can be used as an indicator to understand dietary patterns that may lead to nutrient deficiencies.
- Fibre Intake: The article notes that “Fibre avoidance was notable in CD (52%) and UC (45%).” Tracking fibre intake is an implied indicator, as the conclusion recommends “supervised fibre intake” to maintain intestinal health.
-
Indicators for Target 3.4 (Reduce mortality from NCDs and promote well-being)
- Disease Activity Scores: The article uses “Mayo and HBI scores” to measure disease remission and activity. These clinical scores are direct indicators of how well a non-communicable disease is being managed.
- Quality of Life: The article mentions that dietary restrictions affect “quality of life.” While not quantified with a specific score in the abstract, it is identified as a key outcome, making it an important qualitative indicator for promoting well-being.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 2: Zero Hunger | Target 2.2: By 2030, end all forms of malnutrition… and address the nutritional needs of… older persons and people in vulnerable situations. |
|
| SDG 3: Good Health and Well-being | Target 3.4: By 2030, reduce by one-third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being. |
|
Source: nature.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0