Cardiovascular diseases (CVDs) – World Health Organization (WHO)
Report on Cardiovascular Diseases and the Sustainable Development Agenda
Executive Summary
Cardiovascular diseases (CVDs) represent the foremost global health challenge, posing a significant impediment to the achievement of the 2030 Agenda for Sustainable Development. As the leading cause of mortality worldwide, the CVD epidemic directly undermines SDG 3 (Good Health and Well-being), particularly Target 3.4, which calls for a one-third reduction in premature mortality from non-communicable diseases (NCDs). The burden of CVDs is disproportionately borne by low- and middle-income countries (LMICs), exacerbating inequalities and poverty, thereby challenging progress on SDG 1 (No Poverty) and SDG 10 (Reduced Inequalities). This report outlines the scale of the CVD crisis, its intersection with multiple SDGs, and the strategic interventions required to mitigate its impact.
Global Impact of CVDs: A Threat to SDG 3
The prevalence and mortality associated with CVDs constitute a primary obstacle to ensuring healthy lives and promoting well-being for all. The statistics underscore the urgency of global action in line with SDG 3.
- An estimated 19.8 million deaths were attributed to CVDs in 2022, accounting for 32% of all global deaths.
- Heart attacks and strokes were responsible for 85% of these fatalities.
- A staggering 38% of the 18 million premature deaths (under age 70) from NCDs in 2021 were caused by CVDs, directly challenging the attainment of SDG Target 3.4.
- Critically, over three-quarters of all CVD-related deaths occur in LMICs, highlighting a profound global health inequity.
Classification of Cardiovascular Disorders
CVDs encompass a range of conditions affecting the heart and blood vessels, including:
- Coronary heart disease: Disease of vessels supplying the heart muscle.
- Cerebrovascular disease: Disease of vessels supplying the brain.
- Peripheral arterial disease: Disease of vessels supplying the arms and legs.
- Rheumatic heart disease: Damage to heart muscle and valves resulting from rheumatic fever.
- Congenital heart disease: Malformations of the heart structure present from birth.
- Deep vein thrombosis and pulmonary embolism: Blood clots that form in leg veins and can travel to the heart and lungs.
Multidimensional Risk Factors: A Cross-Cutting SDG Challenge
The drivers of CVDs are complex and interlinked with various environmental, social, and economic factors, reflecting challenges across multiple SDGs.
Behavioural and Dietary Risks
Preventable behavioural factors are major contributors to CVD risk. Addressing them is crucial for public health and sustainable development.
- Unhealthy Diet: Excessive intake of salt, sugars, and fats contributes to obesity and raised blood pressure. This highlights a failure in systems that should support SDG 2 (Zero Hunger), which includes targets for ending all forms of malnutrition.
- Physical Inactivity: Sedentary lifestyles increase CVD risk and are often linked to urban design, a key concern of SDG 11 (Sustainable Cities and Communities).
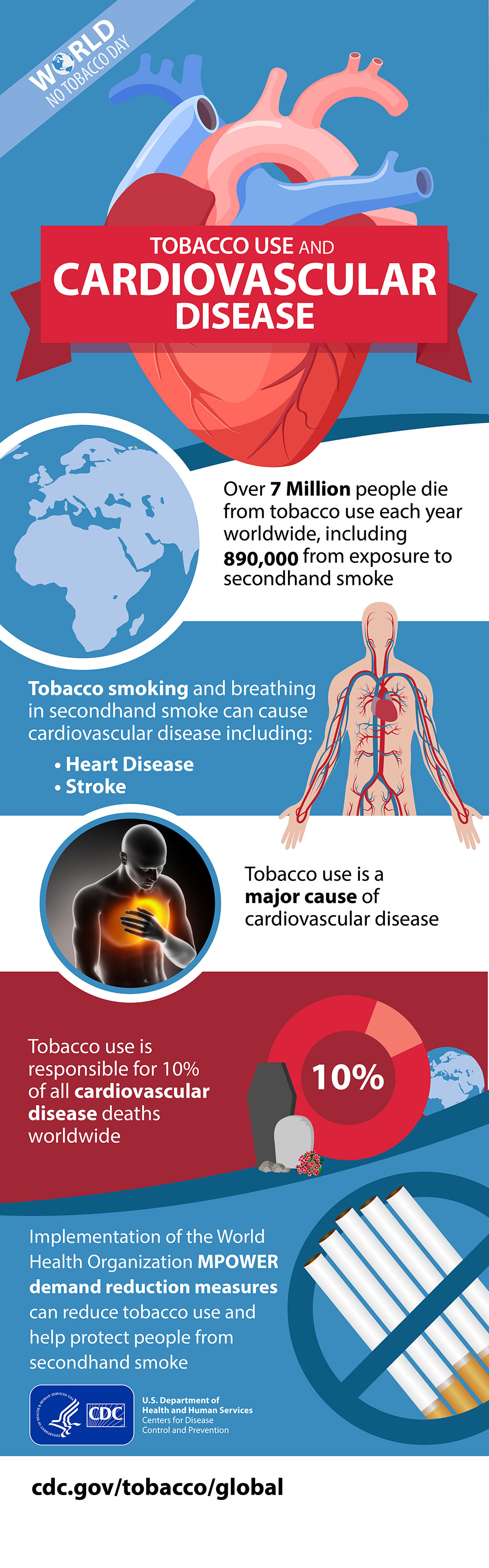
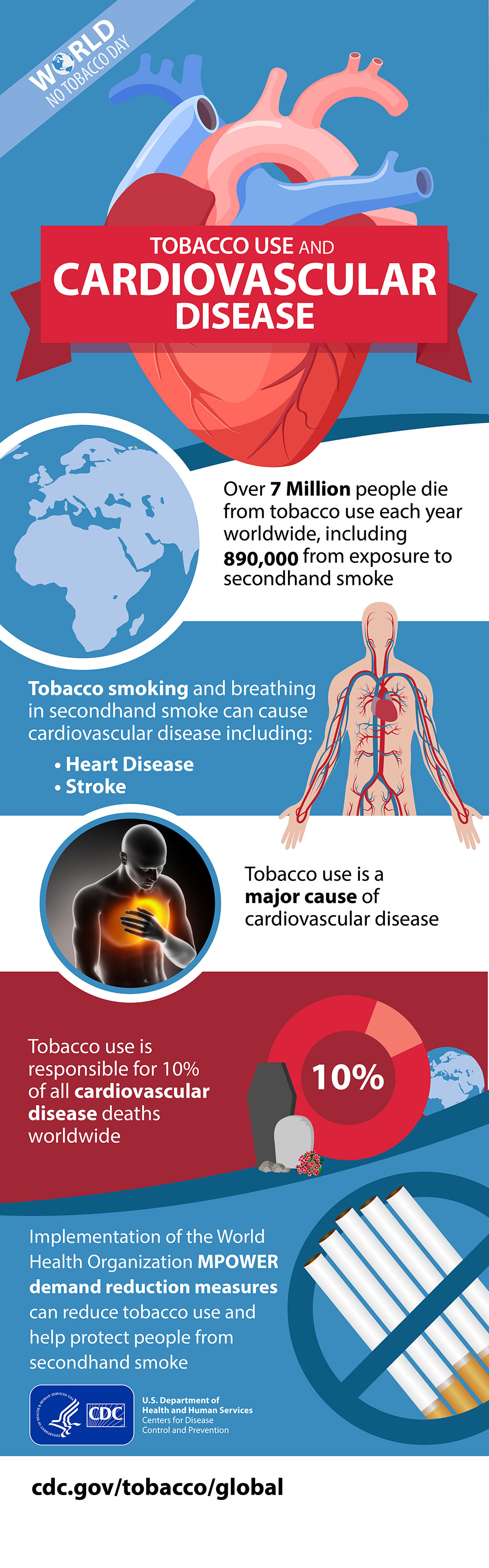
- Tobacco and Harmful Alcohol Use: These are significant risk factors that are explicitly targeted for reduction under SDG 3.
Environmental and Socioeconomic Determinants
Underlying determinants rooted in development patterns significantly influence CVD prevalence.
- Air Pollution: A major environmental risk factor for CVDs, linking public health directly to SDG 11 (Sustainable Cities and Communities) and SDG 13 (Climate Action).
- Poverty and Stress: These factors, central to SDG 1 (No Poverty), are powerful determinants of CVDs, creating a vicious cycle where disease perpetuates poverty.
- Urbanization and Globalization: These trends often promote unhealthy lifestyles and diets, requiring policy interventions aligned with SDG 12 (Responsible Consumption and Production).
CVDs as a Development Crisis: Impact on SDG 1 and SDG 10
The concentration of the CVD burden in LMICs makes it a critical development issue that deepens poverty and inequality.
- Health System Inequity (SDG 10): Individuals in LMICs lack access to primary health care programs for early detection and treatment. This disparity in access to effective health services is a clear manifestation of inequality.
- Contribution to Poverty (SDG 1): At the household level, CVDs lead to catastrophic health spending and high out-of-pocket expenditures, pushing families into poverty.
- Economic Burden: Premature deaths from CVDs occur during individuals’ most productive years, placing a heavy burden on the economies of LMICs and hindering their overall development.
Strategic Interventions to Reduce the CVD Burden
Mitigating the impact of CVDs requires a multi-pronged approach focused on strengthening health systems and ensuring universal access, in direct support of SDG 3, Target 3.8 (Achieve Universal Health Coverage).
Strengthening Primary Health Care for Prevention and Management
- Early Detection: Implement widespread screening in primary care facilities for intermediate risk factors like raised blood pressure, blood glucose, and lipids.
- Counselling and Management: Provide counselling and medication to manage risk factors and prevent acute events like heart attacks and strokes.
- Policy Integration: Create health policies that make healthy choices affordable and available, and improve air quality to create environments conducive to health.
Ensuring Access to Essential Medicines and Technologies
Achieving universal health coverage necessitates the availability of affordable medicines and technologies. Essential medicines for CVD management include:
- Aspirin
- Beta-blockers
- Angiotensin-converting enzyme (ACE) inhibitors
- Statins
Advanced treatments, including surgical operations (e.g., coronary artery bypass) and medical devices (e.g., pacemakers), must also be made accessible and affordable within health systems.
Global Response: Partnerships for the Goals (SDG 17)
International collaboration is essential for supporting countries in their fight against CVDs. The WHO’s response exemplifies SDG 17 (Partnerships for the Goals) by mobilizing global action.
WHO Initiatives and Targets
The WHO’s “Global action plan for the prevention and control of NCDs 2013-2020” established voluntary global targets to reduce premature NCD deaths by 25% by 2025. Key targets directly addressing CVDs include:
- A 25% relative reduction in the global prevalence of raised blood pressure.
- At least 50% of eligible people receive drug therapy and counselling to prevent heart attacks and strokes.
- An 80% availability of affordable basic technologies and essential medicines required to treat major NCDs.
Initiatives like the Global HEARTS Initiative support countries in strengthening CVD prevention and control through primary health care, demonstrating a commitment to collaborative action to achieve the Sustainable Development Goals.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
- The entire article is centered on cardiovascular diseases (CVDs), a major global health issue. It discusses the causes, risk factors, prevention, and treatment of CVDs, directly aligning with the goal of ensuring healthy lives and promoting well-being for all at all ages.
-
SDG 1: No Poverty
- The article establishes a direct link between CVDs and poverty, stating, “At the household level, evidence is emerging that CVDs and other noncommunicable diseases contribute to poverty due to catastrophic health spending and high out-of-pocket expenditure.” This highlights how health issues can trap families in poverty, connecting the issue to SDG 1.
-
SDG 10: Reduced Inequalities
- The article points out significant disparities in the impact of CVDs, noting that “Over three quarters of CVD deaths take place in low- and middle-income countries” and “The poorest people in low- and middle-income countries are most affected.” It also mentions that people in these countries have less access to primary healthcare and equitable services, which is a core concern of SDG 10.
-
SDG 11: Sustainable Cities and Communities
- The article explicitly identifies “air pollution” as an important environmental risk factor for cardiovascular disease. This connects the health issue to the quality of the living environment in human settlements, a key aspect of SDG 11.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
SDG 3: Good Health and Well-being
-
Target 3.4: By 2030, reduce by one-third premature mortality from non-communicable diseases through prevention and treatment.
Support from the article: The text is focused on reducing the burden of CVDs, a primary noncommunicable disease (NCD). It states that “Out of the 18 million premature deaths (under the age of 70) due to noncommunicable diseases in 2021, at least 38% were caused by CVDs.” It also mentions the WHO’s goal “of reducing the number of premature deaths from NCDs by 25% by 2025.” -
Target 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
Support from the article: The article emphasizes that people in low- and middle-income countries “have less access to effective and equitable health care services” and that the solution lies in the “inclusion of cardiovascular disease management interventions in universal health coverage packages.” It also lists essential medicines (aspirin, statins, etc.) and references a WHO target for “80% availability of the affordable basic technologies and essential medicines.” -
Target 3.a: Strengthen the implementation of the World Health Organization Framework Convention on Tobacco Control.
Support from the article: The article identifies “tobacco use” as one of “the most important behavioural risk factors of heart disease and stroke” and mentions “Cessation of tobacco use” as a key preventative measure.
-
Target 3.4: By 2030, reduce by one-third premature mortality from non-communicable diseases through prevention and treatment.
-
SDG 1: No Poverty
-
Target 1.3: Implement nationally appropriate social protection systems and measures for all… and by 2030 achieve substantial coverage of the poor and the vulnerable.
Support from the article: The article’s finding that CVDs contribute to poverty “due to catastrophic health spending and high out-of-pocket expenditure” implies the need for financial risk protection mechanisms, which are a core component of social protection systems under this target.
-
Target 1.3: Implement nationally appropriate social protection systems and measures for all… and by 2030 achieve substantial coverage of the poor and the vulnerable.
-
SDG 10: Reduced Inequalities
-
Target 10.4: Adopt policies, especially fiscal, wage and social protection policies, and progressively achieve greater equality.
Support from the article: The text highlights that “Approximately 80% of the world’s deaths from CVDs occur in low- and middle-income countries” and that the poorest are most affected. It calls for “Health policies that create conducive environments for making healthy choices affordable and available” to address these inequities.
-
Target 10.4: Adopt policies, especially fiscal, wage and social protection policies, and progressively achieve greater equality.
-
SDG 11: Sustainable Cities and Communities
-
Target 11.6: By 2030, reduce the adverse per capita environmental impact of cities, including by paying special attention to air quality.
Support from the article: The article directly names “air pollution” as an “important factor” among environmental risk factors for CVDs, linking urban environmental quality directly to this health outcome.
-
Target 11.6: By 2030, reduce the adverse per capita environmental impact of cities, including by paying special attention to air quality.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
For Target 3.4 (Reduce premature NCD mortality):
- Mortality rate from CVDs: The article states, “An estimated 19.8 million people died from CVDs in 2022, representing approximately 32% of all global deaths.” This is a direct indicator.
- Rate of premature mortality from NCDs: The article mentions “18 million premature deaths (under the age of 70) due to noncommunicable diseases in 2021.” Tracking this number is a direct measure of progress.
- Prevalence of raised blood pressure: The article explicitly cites a WHO target to “Reduce global prevalence of raised blood pressure by 25% between 2010 and 2025,” which serves as a specific indicator.
- Prevalence of behavioral risk factors: The article implies tracking rates of “tobacco use, unhealthy diet… physical inactivity, harmful use of alcohol” as indicators for prevention efforts.
-
For Target 3.8 (Universal Health Coverage):
- Availability of essential medicines and technologies: The article cites a specific WHO target: “80% availability of the affordable basic technologies and essential medicines… in both public and private facilities.” This is a measurable indicator.
- Access to treatment and counseling: The article includes a WHO target that “At least 50% of eligible people should receive drug therapy and counselling… to prevent heart attacks and strokes by 2025.”
- Rate of catastrophic health spending: The article implies this indicator by mentioning that CVDs lead to poverty through “catastrophic health spending and high out-of-pocket expenditure.”
-
For Target 11.6 (Reduce environmental impact of cities):
- Level of air pollution: By identifying “air pollution” as a key environmental risk factor, the article implies that measuring air quality (e.g., particulate matter concentrations) is a relevant indicator for tracking progress in reducing this risk.
4. Summary Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators Identified in the Article |
|---|---|---|
| SDG 3: Good Health and Well-being |
3.4: Reduce premature mortality from NCDs.
3.8: Achieve universal health coverage and access to essential medicines. 3.a: Strengthen tobacco control. |
– Mortality rate from CVDs (19.8 million in 2022). – Number of premature deaths from NCDs (18 million in 2021). – Global prevalence of raised blood pressure (Target: 25% reduction). – Percentage of eligible people receiving drug therapy and counseling (Target: 50%). – Percentage availability of affordable basic technologies and essential medicines (Target: 80%). – Prevalence of tobacco use. |
| SDG 1: No Poverty | 1.3: Implement social protection systems. | – Incidence of catastrophic health spending and high out-of-pocket expenditure due to CVDs. |
| SDG 10: Reduced Inequalities | 10.4: Adopt policies to achieve greater equality. | – Proportion of CVD deaths occurring in low- and middle-income countries (Over 75%). – Access to equitable health care services for the poorest populations. |
| SDG 11: Sustainable Cities and Communities | 11.6: Reduce the adverse environmental impact of cities, focusing on air quality. | – Level of air pollution (identified as a key environmental risk factor). |
Source: who.int
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0


























;Resize=805#)