Food Is Medicine and the Future of Care Delivery – Food Tank

Report on the “Food Is Medicine” Initiative and its Alignment with Sustainable Development Goals
Executive Summary
The “Food Is Medicine” initiative in the United States represents a significant strategic shift in healthcare, aiming to integrate nutrition-based interventions into standard medical practice. This approach directly addresses several United Nations Sustainable Development Goals (SDGs), primarily SDG 3 (Good Health and Well-being) by combating diet-related non-communicable diseases. The initiative’s focus on food access, education, and multi-sector collaboration also contributes to SDG 2 (Zero Hunger), SDG 4 (Quality Education), SDG 10 (Reduced Inequalities), and SDG 17 (Partnerships for the Goals). This report analyzes the current landscape, challenges, and strategic pathways for scaling this initiative, emphasizing its potential to advance the global sustainability agenda.
The Challenge: A Disconnect Between Nutrition and Healthcare
A critical gap exists within the U.S. healthcare system that impedes progress toward SDG 3. Diet-related illnesses are the leading cause of death, yet medical education provides insufficient training in nutrition.
- U.S. medical schools dedicate, on average, fewer than 20 hours to nutrition education across a four-year curriculum.
- This educational deficit limits the capacity of physicians to address the root causes of many chronic diseases, hindering efforts to reduce premature mortality from non-communicable diseases as targeted by SDG 3.4.
The “Food Is Medicine” Movement: A Strategy for Sustainable Health
The “Food Is Medicine” concept is gaining significant momentum, reframing nutrition as a critical tool for health maintenance, disease prevention, and treatment. This approach is foundational to achieving sustainable health outcomes.
Core Interventions and SDG Alignment
The initiative’s primary interventions are designed to create a more holistic and equitable healthcare system.
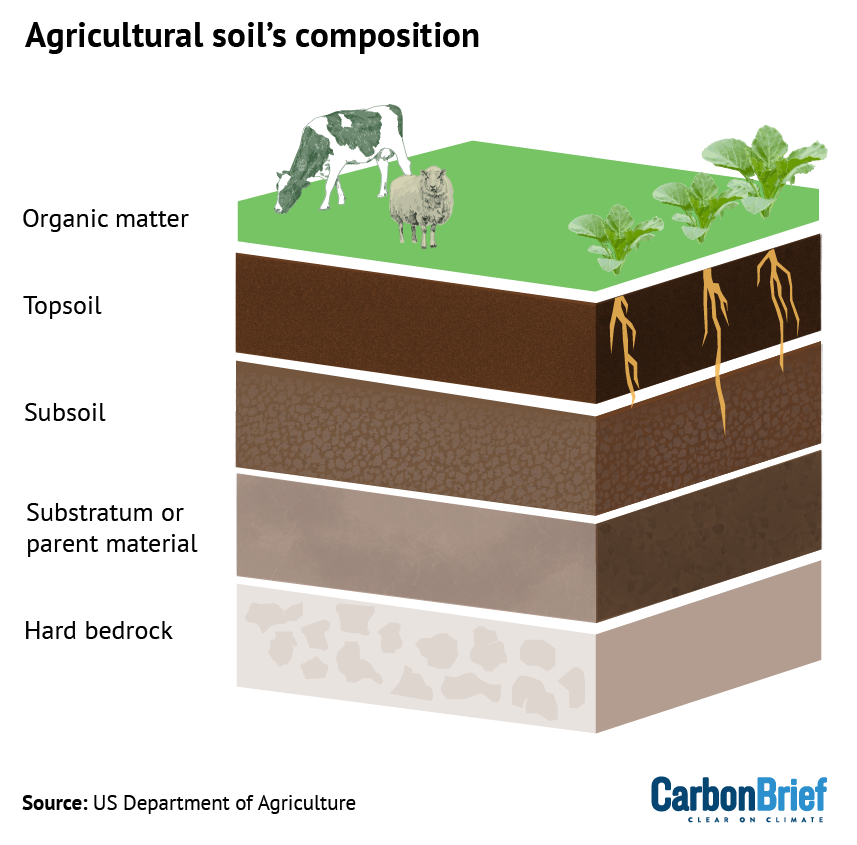
- Medically Tailored Meals and Produce Prescriptions: These interventions directly provide nutritious food to patients, addressing immediate health needs (SDG 3) while also tackling food insecurity and improving access to nutritious food (SDG 2).
- Enrollment in Assistance Programs: Proactively connecting patients with programs like SNAP and WIC helps to reduce hunger and malnutrition, directly supporting the targets of SDG 2 and reducing health inequalities (SDG 10).
- Nutrition Education: Empowering patients with knowledge about healthy eating promotes long-term well-being and preventative health, a core tenet of SDG 3.
Fostering Multi-Stakeholder Collaboration for the Goals (SDG 17)
The scaling of “Food Is Medicine” is being driven by robust partnerships across the public and private sectors, a clear demonstration of SDG 17 in action.
- Nearly US$10 billion has been committed by various organizations to combat diet-related disease and hunger.
- The Food Is Medicine National Network of Excellence, founded by Tufts University and Kaiser Permanente, unites major healthcare organizations like CVS Health, Elevance Health, and Geisinger to standardize and integrate food-based interventions.
- Corporate entities like Instacart are launching mission-driven arms to improve nutrition access and education, showcasing private sector engagement in public health goals.
Strategic Imperatives for System-Wide Integration
Reforming Medical Education to Achieve SDG 4
A primary pathway to systemic change is through the enhancement of medical training, aligning with SDG 4 (Quality Education) to equip future health professionals with necessary skills.
Case Study: Kaiser Permanente Bernard J. Tyson School of Medicine
- Integrated Curriculum: Nutrition is woven throughout the curriculum, linking it to metabolic disorders, heart disease, and pregnancy, rather than treating it as an isolated topic.
- Holistic Training: Students receive instruction on food insecurity, scientific approaches to nutrition, and policy levers for change.
- Specialized Electives: An intensive 120-hour culinary medicine elective provides deep knowledge in nutrition and culinary literacy, preparing physicians to offer practical, food-based counseling.
Addressing Health Inequalities (SDG 10) and Hunger (SDG 2)
Effective implementation requires a patient-centered approach that acknowledges and addresses the social determinants of health, which is crucial for reducing inequalities.
- Care teams must be trained to consider variables such as cooking ability, grocery store accessibility, food insecurity, and cultural foodways.
- Recognizing that food insecurity is a top social health need, physicians must be equipped to connect patients with assistance programs like SNAP, WIC, and Summer EBT, directly contributing to the targets of SDG 2.
Conclusion and Outlook
The “Food Is Medicine” initiative offers a promising, evidence-based framework for transforming the U.S. healthcare system. By investing in the education of future physicians and fostering strong multi-stakeholder partnerships, this movement is on a path to being fully integrated within the next 5 to 10 years. This reorientation will not only save lives and reduce healthcare costs but will also make substantial contributions to achieving multiple Sustainable Development Goals, creating a healthier, more equitable, and sustainable future for generations to come.
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 2: Zero Hunger
- The article directly addresses food access and nutrition, which are central to SDG 2. It mentions tackling “hunger” and “food insecurity,” which it identifies as “the top social health need that Americans experience.” It also discusses interventions like “prescriptions for produce” and enrollment in assistance programs such as “SNAP, WIC, and Summer EBT” to ensure people have access to nutritious food.
-
SDG 3: Good Health and Well-being
- This is the primary SDG connected to the article. The entire piece revolves around improving health outcomes by integrating nutrition into healthcare. It highlights that “diet-related disease remains the leading cause of death in the United States” and presents the “Food Is Medicine” concept as a strategy for “preventing and managing disease,” reducing “health care costs,” and ultimately “improving and saving lives.”
-
SDG 4: Quality Education
- The article identifies a critical “educational gap” in the training of physicians. It states that “U.S. medical schools currently devote, on average, fewer than 20 hours to nutrition education.” A core part of the proposed solution is to reform medical education by making “nutrition curriculum and food security support a core component of medical education” to ensure future doctors have the necessary knowledge and skills.
-
SDG 17: Partnerships for the Goals
- The article emphasizes the importance of collaboration across different sectors. It provides concrete examples of “public-private and civil society partnerships,” such as the “Food Is Medicine National Network of Excellence,” which brings together academic institutions (Tufts), nonprofit health systems (Kaiser Permanente), and major private healthcare companies (CVS Health, Elevance Health, etc.). It also mentions a commitment of “nearly US$10 billion” from “Private and public sector organizations.”
2. What specific targets under those SDGs can be identified based on the article’s content?
-
SDG 2: Zero Hunger
-
Target 2.1: End hunger and ensure access to safe, nutritious and sufficient food.
- The article supports this target by focusing on solutions to “food insecurity.” It advocates for interventions like “prescriptions for produce” and better utilization of “assistance programs like SNAP, WIC, and Summer EBT” to ensure vulnerable populations have access to healthy food.
-
Target 2.2: End all forms of malnutrition.
- The article’s central theme of using “Food Is Medicine” to combat “diet-related disease” directly relates to ending malnutrition, which includes both undernutrition and the effects of poor diets. It discusses providing “medically tailored meals” and addressing “vitamin and mineral deficiencies” as part of a holistic healthcare approach.
-
-
SDG 3: Good Health and Well-being
-
Target 3.4: Reduce by one third premature mortality from non-communicable diseases (NCDs).
- The article directly addresses this target by aiming to reverse the trend of “diet-related disease” (a primary category of NCDs) being the “leading cause of death in the United States.” The entire “Food Is Medicine” initiative is framed as a preventative strategy to “improve and save lives” from these chronic conditions.
-
Target 3.d: Strengthen the capacity for early warning, risk reduction and management of national health risks.
- The article argues for strengthening the U.S. healthcare system’s capacity to manage the risks of diet-related diseases. This is achieved by training “the next generation of physicians” in nutrition, enabling them to provide “practical counseling on meal planning and healthy eating,” thereby preventing illness before it becomes severe.
-
-
SDG 4: Quality Education
-
Target 4.7: Ensure all learners acquire knowledge and skills needed for sustainable development and sustainable lifestyles.
- The article critiques the current “limited exposure” of medical students to nutrition (“fewer than 20 hours”) and advocates for a new educational model. It highlights the Kaiser Permanente medical school, which provides “120 hours” of instruction in a culinary medicine elective, as an example of equipping learners (future doctors) with the skills to promote healthy and sustainable lifestyles among their patients.
-
-
SDG 17: Partnerships for the Goals
-
Target 17.17: Encourage and promote effective public, public-private and civil society partnerships.
- The article showcases this target in action by describing the “Food Is Medicine National Network of Excellence,” a collaboration between “Tufts Friedman School of Nutrition Science and Policy,” “Kaiser Permanente,” and several large healthcare companies. It also mentions partnerships between Instacart and Kaiser Permanente and the nearly “US$10 billion” committed by various “Private and public sector organizations.”
-
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
SDG 2: Zero Hunger
-
Prevalence of food insecurity (related to Indicator 2.1.2)
- The article implies this indicator by stating that “food insecurity is consistently the top social health need that Americans experience.” Measuring the reduction in the prevalence of food insecurity would be a key metric for the success of programs like SNAP, WIC, and produce prescriptions.
-
-
SDG 3: Good Health and Well-being
-
Mortality rate from diet-related NCDs (related to Indicator 3.4.1)
- The article states that “diet-related disease remains the leading cause of death.” A direct measure of progress would be a reduction in the mortality rate from these diseases, which include heart disease and metabolic disorders mentioned in the text.
-
-
SDG 4: Quality Education
-
Hours of nutrition education in medical school curricula (related to Indicator 4.7.1)
- The article provides a clear, quantifiable indicator for progress in education. It contrasts the current average of “fewer than 20 hours” with model programs that offer “120 hours” in specialized electives. Tracking the increase in required and elective nutrition education hours across medical schools would measure progress toward this goal.
-
-
SDG 17: Partnerships for the Goals
-
Amount of financial commitment to partnerships (related to Indicator 17.17.1)
- The article provides a direct, quantifiable indicator by stating that “Private and public sector organizations have committed nearly US$10 billion to change the trajectory of diet-related disease and hunger in the U.S.” This figure serves as a baseline to measure future investment and commitment.
-
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators Identified in Article |
|---|---|---|
| SDG 2: Zero Hunger | Target 2.1: End hunger and ensure access to safe, nutritious and sufficient food. | Prevalence of food insecurity (Implied by the statement that it is the “top social health need”). |
| Target 2.2: End all forms of malnutrition. | Implementation of interventions like “medically tailored meals” to address diet-related disease. | |
| SDG 3: Good Health and Well-being | Target 3.4: Reduce premature mortality from non-communicable diseases (NCDs). | Reduction in mortality from “diet-related disease,” which is the “leading cause of death.” |
| Target 3.d: Strengthen capacity for management of national health risks. | Number of physicians trained in “Food Is Medicine” strategies to prevent and manage diet-related disease. | |
| SDG 4: Quality Education | Target 4.7: Ensure all learners acquire knowledge and skills for sustainable lifestyles. | Number of hours dedicated to nutrition in medical school curricula (contrasting the current “fewer than 20 hours” with model programs). |
| SDG 17: Partnerships for the Goals | Target 17.17: Encourage effective public, public-private and civil society partnerships. | Amount of financial commitment from partnerships (Directly stated as “nearly US$10 billion”). |
Source: foodtank.com

What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0