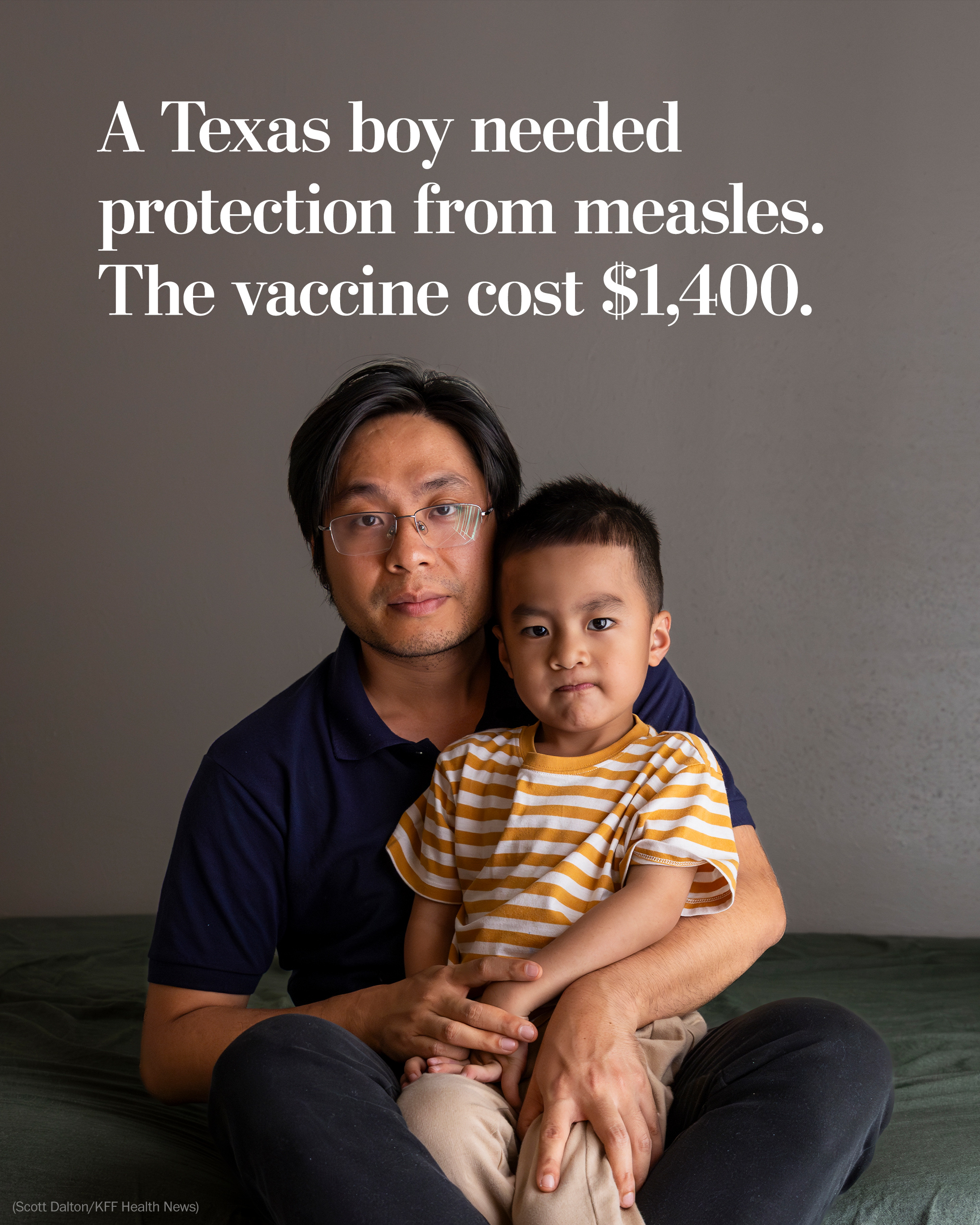
A Texas boy needed protection from measles. The vaccine cost $1,400. – The Washington Post
Report on Measles Vaccination Coverage and Billing Challenges Amid West Texas Outbreak
Introduction
During the early stages of the West Texas measles outbreak, concerns arose regarding vaccination coverage, particularly for children partially vaccinated. This report highlights the case of the Nguyen family from Galveston, Texas, emphasizing the challenges faced in accessing affordable immunizations amid a public health crisis. The analysis underscores the relevance of Sustainable Development Goals (SDGs), particularly SDG 3: Good Health and Well-being, and SDG 10: Reduced Inequalities.
Background of the Measles Outbreak and Vaccination Protocols
- The measles vaccine was first licensed in 1963 and later combined into the MMR (measles, mumps, rubella) vaccine in 1971.
- The MMRV vaccine additionally covers chickenpox (varicella).
- Standard vaccination schedule includes a first dose between 12-15 months and a second dose between ages 4-6.
- During outbreaks, earlier vaccination may be recommended to increase immunity.
- Over 1,200 measles cases were reported in the U.S. during the outbreak, with 750 in Texas; 95% of cases involved unvaccinated or unknown vaccination status individuals.
Case Study: Nguyen Family’s Vaccination Experience
- Thang Nguyen, a public health postdoctoral fellow, took his family to the University of Texas Medical Branch (UTMB) clinic for immunizations amid the outbreak.
- His 4-year-old son received the MMRV vaccine plus additional immunizations for tetanus, diphtheria, whooping cough, and influenza.
- The twin daughters received other recommended vaccines.
- Nguyen was assured by clinic staff that insurance would cover the immunizations.
- Subsequently, the family received medical bills totaling nearly $5,000, including $1,422 for the MMRV vaccine alone.
Challenges in Insurance Coverage and Billing
- The family’s insurance plan, purchased through an international broker, did not cover immunizations or preventive care.
- The Vaccines for Children Program, a federally funded initiative aligned with SDG 3 to ensure equitable access to vaccines, was initially not offered to the family.
- UTMB’s chargemaster listed vaccine prices significantly higher than CDC private sector estimates ($1,400 vs. approximately $278).
- Errors in insurance information entry and billing led to improper charges.
- International students on temporary visas are exempt from Affordable Care Act (ACA) requirements, limiting access to comprehensive coverage.
Implications for Sustainable Development Goals
- SDG 3 (Good Health and Well-being): Ensuring access to affordable vaccines is critical for controlling outbreaks and promoting health equity.
- SDG 10 (Reduced Inequalities): The case illustrates disparities in healthcare access for immigrant families and those with non-ACA-compliant insurance plans.
- SDG 17 (Partnerships for the Goals): Collaboration between healthcare providers, insurers, and public health programs is essential to address coverage gaps.
Resolution and Recommendations
- Following intervention, UTMB applied a 50% self-pay discount and subsequently waived vaccine costs for the Nguyen family, reducing the bill to approximately $203.
- Recommendations for patients and policymakers include:
- Verifying insurance coverage for preventive services before receiving care.
- Utilizing public health vaccination programs, such as the Vaccines for Children Program, which provide free immunizations to eligible children.
- Advocating for policy reforms to extend ACA protections to international students and other vulnerable populations.
- Encouraging transparency in medical pricing and billing practices to prevent excessive charges.
Conclusion
The Nguyen family’s experience during the measles outbreak highlights systemic challenges in vaccine accessibility and affordability in the United States. Addressing these issues aligns with the Sustainable Development Goals by promoting health equity, reducing inequalities, and strengthening healthcare systems. Enhanced coordination among healthcare providers, insurers, and public health programs is vital to ensure that all populations, including immigrants and those with limited insurance coverage, receive essential preventive care without financial hardship.
1. Sustainable Development Goals (SDGs) Addressed or Connected
- SDG 3: Good Health and Well-being
- The article focuses on vaccination, disease prevention, and access to healthcare services, which are central to SDG 3.
- It highlights issues related to measles outbreaks, immunization coverage, and healthcare affordability.
- SDG 1: No Poverty
- The financial burden of medical bills and lack of insurance coverage for preventive care relate to poverty alleviation and reducing economic barriers to health services.
- SDG 10: Reduced Inequalities
- The article discusses disparities in healthcare access for international students and uninsured or underinsured populations, highlighting inequality issues.
- SDG 17: Partnerships for the Goals
- References to federal programs like the Vaccines for Children Program and public health departments indicate the role of partnerships in achieving health goals.
2. Specific Targets Under Those SDGs Identified
- SDG 3: Good Health and Well-being
- Target 3.3: End epidemics of communicable diseases such as measles by increasing immunization coverage.
- Target 3.8: Achieve universal health coverage, including access to quality essential healthcare services and affordable medicines and vaccines.
- SDG 1: No Poverty
- Target 1.3: Implement social protection systems to reduce the financial burden of healthcare on vulnerable populations.
- SDG 10: Reduced Inequalities
- Target 10.2: Empower and promote social, economic, and political inclusion of all, irrespective of status, including migrants and temporary residents.
- SDG 17: Partnerships for the Goals
- Target 17.17: Encourage effective public, public-private, and civil society partnerships to support health programs like vaccination campaigns.
3. Indicators Mentioned or Implied to Measure Progress
- Immunization Coverage Rates
- The article mentions the percentage of measles cases occurring in unvaccinated individuals (95%), implying the use of vaccination coverage as an indicator.
- Incidence of Measles Cases
- Number of reported measles cases (over 1,200 in the U.S., 750 in Texas) serves as an indicator of disease control progress.
- Health Insurance Coverage
- Coverage of preventive services like immunizations under health insurance plans is implied as an indicator of access to healthcare.
- Cost of Vaccines and Out-of-Pocket Expenses
- Financial barriers and billing errors highlight the importance of monitoring affordability and financial protection indicators.
- Utilization of Public Health Programs
- Participation in programs like the Vaccines for Children Program is an indicator of equitable access to immunizations.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being |
|
|
| SDG 1: No Poverty |
|
|
| SDG 10: Reduced Inequalities |
|
|
| SDG 17: Partnerships for the Goals |
|
|
Source: kffhealthnews.org

What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0