Healthcare seeking behavior and antibiotic use for diarrhea among children in rural Bangladesh before seeking care at a healthcare facility – Nature
Report on Healthcare Seeking Behavior and Antibiotic Use for Childhood Diarrhea in Rural Bangladesh
1.0 Introduction and Context
This report analyzes care-seeking behaviors and antibiotic usage for childhood diarrhea in rural Bangladesh, based on a study of 8,294 diarrheal episodes in children aged 1-59 months. The findings are critically examined through the lens of the United Nations Sustainable Development Goals (SDGs), particularly SDG 3 (Good Health and Well-being). The analysis reveals significant challenges to achieving global targets related to child mortality (SDG 3.2), universal health coverage (SDG 3.8), and the management of global health risks like antimicrobial resistance (AMR) (SDG 3.d).
2.0 Key Findings on Treatment Practices and Care-Seeking
The study reveals treatment patterns that deviate significantly from World Health Organization (WHO) guidelines. These practices pose direct risks to child health and undermine progress toward the SDGs by contributing to the global health crisis of AMR.
2.1 Antibiotic and Medication Usage Statistics
- Widespread Antibiotic Overuse: 55% of children received antibiotics, while only 6% presented with dysentery, the primary clinical indication for such treatment. This practice directly undermines SDG Target 3.d by fueling the emergence of AMR.
- Non-Prescription Access: An alarming 77% of antibiotics were obtained from local pharmacies without a formal prescription from a qualified health professional. This highlights weak regulatory oversight and a significant barrier to achieving SDG Target 3.8 (Universal Health Coverage).
- Suboptimal Adherence to Recommended Treatment:
- While 85% of children received Oral Rehydration Solution (ORS), only 7% received the complete WHO-recommended treatment of ORS and zinc without the addition of unnecessary antibiotics.
- This gap in appropriate care directly impacts progress towards SDG Target 3.2 (End preventable deaths of children under 5), as correct management is crucial for reducing diarrhea-related mortality and its contribution to malnutrition (SDG 2: Zero Hunger).
- Paradoxical Hospitalization Rates: Children who received antibiotics prior to formal hospital care had a significantly higher rate of hospitalization (20%) compared to those who did not (13%). This suggests that inappropriate antibiotic use may delay effective treatment and worsen outcomes, hindering the goals of SDG 3.
2.2 Care-Seeking Behaviors and Influencing Factors
Caregiver decisions were shaped by a combination of socio-economic and systemic factors, revealing critical gaps in health systems and public awareness that impede the achievement of the SDGs.
- Reliance on the Informal Healthcare Sector: The primary source for antibiotics was local pharmacies, a practice driven by:
- A perception that antibiotics lead to faster recovery.
- Traditional practices and established trust in pharmacy-provided treatments over formal systems.
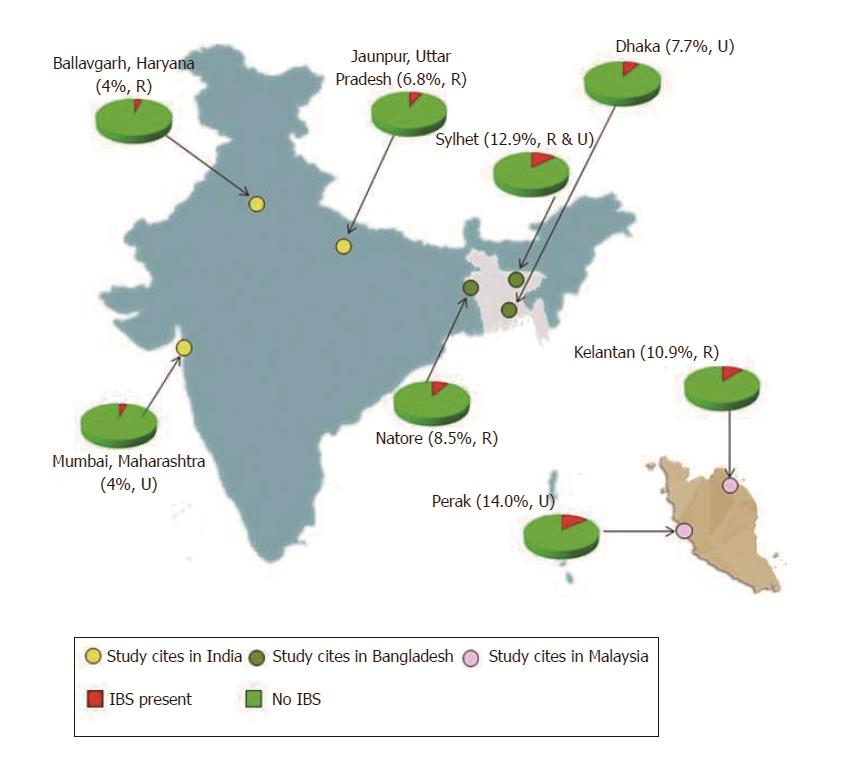
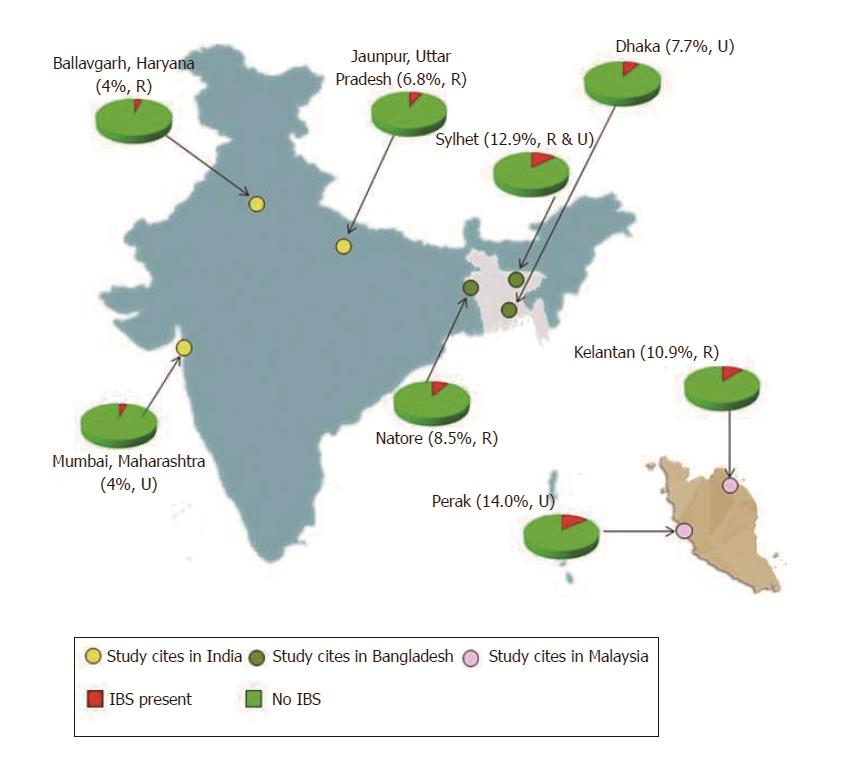
- Barriers to Formal Healthcare Access: Geographic distance to a formal healthcare facility was a significant determinant of antibiotic use. Children from more distant unions demonstrated higher rates of antibiotic consumption, highlighting a clear inequality in healthcare access. This disparity is a core concern of SDG 10 (Reduced Inequalities) and a major obstacle to achieving SDG 3.8.
3.0 Implications for Sustainable Development Goals (SDGs)
The study’s findings have profound and interconnected implications for several SDGs, extending beyond immediate health outcomes to issues of inequality and responsible consumption.
3.1 SDG 3: Good Health and Well-being
- Target 3.2 (End Preventable Child Deaths): The overuse of antibiotics and underuse of zinc for a leading childhood illness directly impede efforts to reduce preventable child mortality.
- Target 3.8 (Universal Health Coverage): The widespread reliance on unregulated pharmacies for primary care demonstrates a failure in providing accessible, affordable, and quality formal healthcare, which are the cornerstones of UHC.
- Target 3.d (Combat Health Crises): The injudicious use of antibiotics is a primary driver of Antimicrobial Resistance (AMR), an escalating global health crisis. The study quantifies this driver at a local level, showing how community practices contribute to a global threat.
3.2 Broader SDG Linkages
- SDG 10 (Reduced Inequalities): The correlation between distance from a health facility and higher rates of inappropriate antibiotic use illustrates a stark socio-economic and geographic divide in healthcare access and quality.
- SDG 12 (Responsible Consumption and Production): The widespread, non-prescription sale and use of antibiotics represent a pattern of irresponsible consumption of pharmaceuticals. This has severe public health and environmental consequences, including the proliferation of drug-resistant pathogens.
4.0 Conclusion and Recommendations for SDG Alignment
The significant overuse of antibiotics for childhood diarrhea in rural Bangladesh, driven by inadequate access to formal healthcare and low public awareness, poses a direct threat to achieving multiple Sustainable Development Goals. The association of initial antibiotic use with higher subsequent hospitalization rates underscores the ineffectiveness and potential harm of current community practices.
To align with the 2030 Agenda for Sustainable Development, the following actions are imperative:
- Strengthen Health Systems (SDG 3.8, SDG 10): Enhance access to and trust in formal healthcare facilities, particularly in remote and underserved areas, to reduce reliance on informal providers.
- Enforce Regulations (SDG 3.d, SDG 12): Implement and strictly enforce laws governing the sale of over-the-counter antibiotics to curb irresponsible consumption and combat the spread of AMR.
- Increase Public Awareness (SDG 3.2): Launch targeted public health campaigns to educate caregivers on the correct management of diarrhea (emphasizing ORS and zinc) and the specific dangers of unnecessary antibiotic use for both individual children and public health.
Which SDGs are addressed or connected to the issues highlighted in the article?
SDG 3: Good Health and Well-being
The article is fundamentally centered on public health issues, making SDG 3 the most relevant goal. The analysis connects to several core aspects of ensuring healthy lives and promoting well-being for all ages.
- Child Mortality and Morbidity: The article directly addresses childhood diarrhea, which it identifies as “the third leading cause of death in children under five years old globally” and a principal cause of morbidity and malnutrition. This aligns with the SDG 3 objective of reducing child mortality.
- Communicable Diseases: Diarrhea is a communicable disease, and the article discusses its treatment, prevention of its complications, and the challenges in its management, which is a core component of combating such diseases.
- Antimicrobial Resistance (AMR): A significant portion of the article is dedicated to the “overuse of antibiotics,” which “notably increases antibiotic resistance.” AMR is highlighted as a “significant public health threat” with severe health and economic consequences, a critical global health risk that SDG 3 aims to address.
- Access to Healthcare and Medicines: The study investigates “care-seeking behavior,” including the reliance on local pharmacies versus formal healthcare facilities, the influence of “distance to a healthcare facility,” and the use of essential medicines like Oral Rehydration Solution (ORS), zinc, and antibiotics. This directly relates to achieving universal health coverage.
What specific targets under those SDGs can be identified based on the article’s content?
SDG 3: Good Health and Well-being
-
Target 3.2: By 2030, end preventable deaths of newborns and children under 5 years of age.
The article’s focus on diarrhea, a leading cause of death in children under five, directly relates to this target. The study analyzes treatment compliance with WHO guidelines (ORS, zinc) which are designed to reduce diarrhea-related childhood mortality. The finding that children who received antibiotics before hospital care had a “significantly higher rate of hospitalization” (20% vs. 13%) underscores the link between improper treatment and severe morbidity, a precursor to mortality.
-
Target 3.3: By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.
Diarrhea is a major communicable and often water-borne disease. The article’s entire premise is to study the management of diarrheal episodes in children in Bangladesh. It examines the effectiveness and appropriateness of treatments being used to combat this disease, highlighting a significant gap between WHO guidelines and actual practice, which is a major barrier to controlling the disease’s impact.
-
Target 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
This target is addressed through the article’s analysis of care-seeking patterns. It reveals issues with access to quality healthcare, as “77% of the antibiotics were obtained from a local pharmacy without a prescription.” The reasons cited, such as “distance to a healthcare facility” and “faith in seeking care at pharmacies,” point to barriers in accessing formal and quality healthcare services. The discussion on the use of ORS, zinc, and antibiotics is a direct examination of access to and proper use of essential medicines.
-
Target 3.d: Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks.
The article identifies the “global rise in antimicrobial resistance (AMR)” as a major public health threat. The study’s finding that 55% of children received antibiotics, mostly for watery diarrhea where it is not recommended, is a clear indicator of a systemic problem driving this global health risk. The conclusion calls for “strengthening laws and regulations on the sale of over-the-counter antibiotics,” which is a direct recommendation for strengthening national capacity to manage the risk of AMR.
Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
SDG 3: Good Health and Well-being
The article provides specific quantitative data that can serve as direct or proxy indicators for the identified targets.
-
Indicators for Target 3.2 (End child mortality):
- Under-5 mortality rate (Implied): While not stating a mortality rate, the article addresses a leading cause of it. The hospitalization rate is used as a proxy for severe morbidity that can lead to death. The data shows a “significantly higher rate of hospitalization” (20%) in children who received antibiotics compared to those who did not (13%).
-
Indicators for Target 3.3 (Combat communicable diseases):
- Incidence of diarrhea: The study is based on the analysis of “8294 diarrheal episodes,” which serves as a measure of disease incidence in the study population.
- Proportion of population with access to appropriate treatment: The article provides clear metrics on treatment practices for diarrhea. For example, “while 85% of the children received ORS, only 7% received zinc and ORS without antibiotics,” indicating that a very small portion of children received the complete, recommended treatment without inappropriate additions.
-
Indicators for Target 3.8 (Universal health coverage):
- Coverage of essential health services: The article measures the source of care, showing a heavy reliance on informal providers. The fact that “76.76% of the children, sought care at a local pharmacy” for antibiotics indicates a gap in the coverage of formal, professional health services.
- Access to essential medicines: The article provides percentages for the use of key medicines: 85.27% received ORS, but only 35.17% received ORS and zinc together. This measures the population’s access to and use of essential medicines for diarrhea.
- Access to healthcare facilities: The article implies this is a barrier, noting that “distance to a healthcare facility” was a reason for seeking care at a pharmacy and that children from distant unions had higher antibiotic consumption rates (e.g., 70.55%).
-
Indicators for Target 3.d (Manage health risks):
- Rate of inappropriate antibiotic use: This is a key indicator for the risk of AMR. The article states that “55% of the study children received antibiotics, while only 6% had dysentery,” providing a quantifiable measure of overuse.
- Proportion of antibiotics sold without a prescription: The finding that “77% of the antibiotics were obtained from a local pharmacy without a prescription” is a direct indicator of weak regulation and control over antimicrobials, a key driver of AMR.
SDGs, Targets and Indicators Table
| SDGs | Targets | Indicators Identified in the Article |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.2: End preventable deaths of children under 5. |
|
| SDG 3: Good Health and Well-being | 3.3: Combat communicable diseases. |
|
| SDG 3: Good Health and Well-being | 3.8: Achieve universal health coverage and access to quality essential healthcare and medicines. |
|
| SDG 3: Good Health and Well-being | 3.d: Strengthen capacity to manage national and global health risks. |
|
Source: nature.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0