Hepatitis B – World Health Organization (WHO)
Report on the Global Impact of Hepatitis B in the Context of the Sustainable Development Goals
The Challenge to SDG 3: Good Health and Well-being
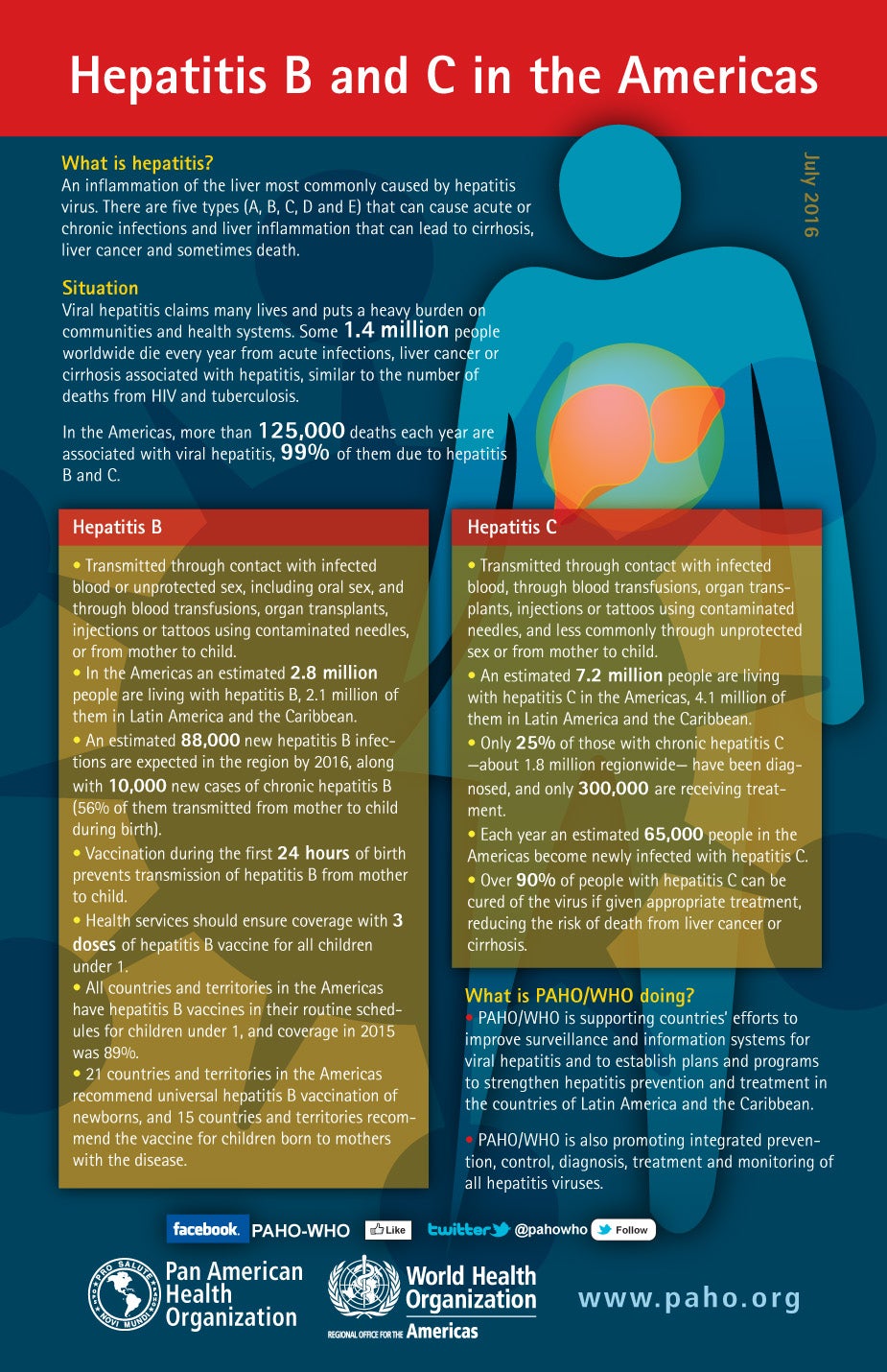
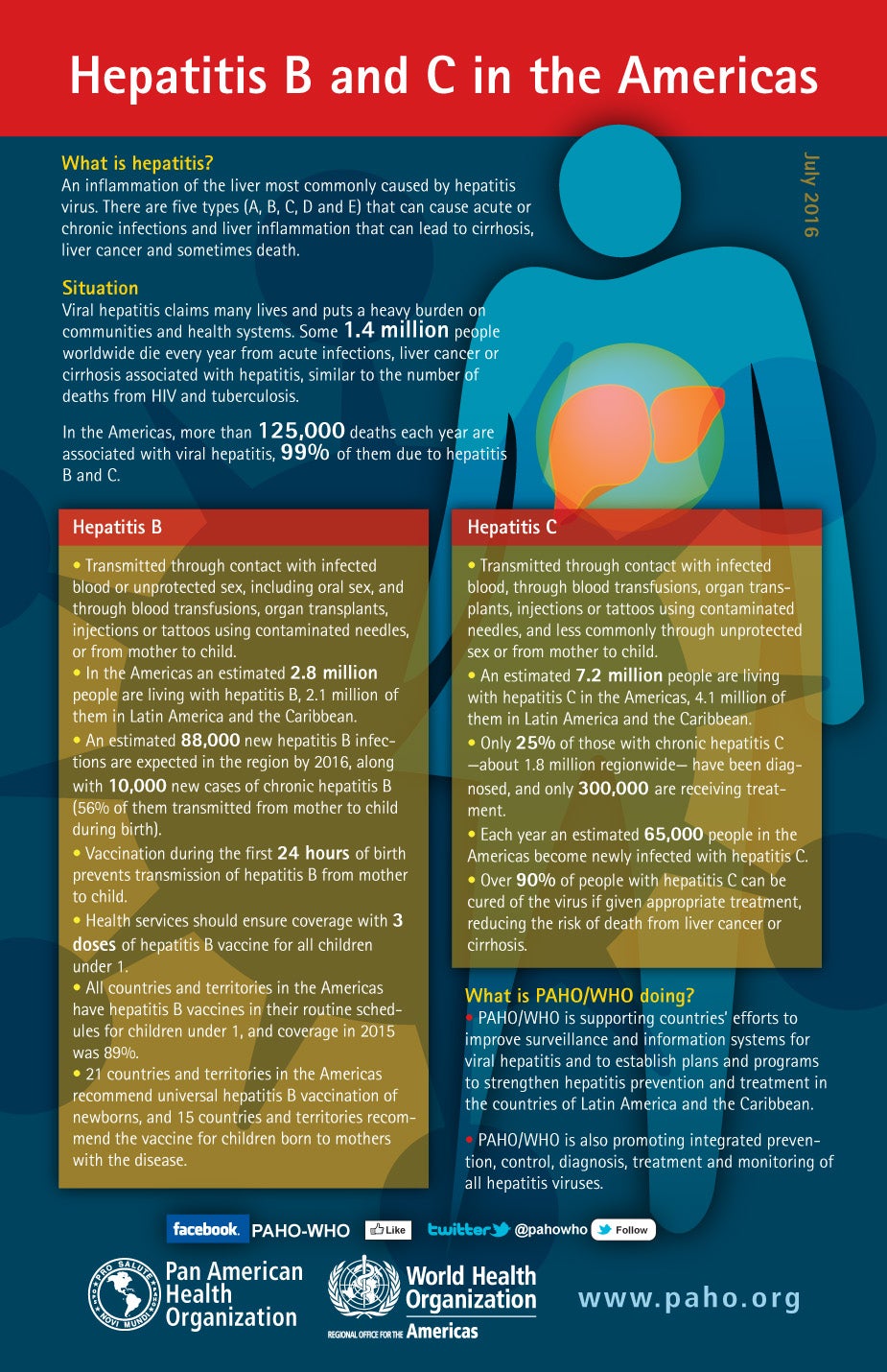
Hepatitis B, a viral liver infection, presents a significant obstacle to achieving Sustainable Development Goal 3 (SDG 3), which aims to ensure healthy lives and promote well-being for all at all ages. The disease, which can be acute or chronic, leads to high rates of mortality from cirrhosis and liver cancer, directly undermining SDG Target 3.4, which calls for a one-third reduction in premature mortality from non-communicable diseases. The global burden of Hepatitis B underscores the urgent need for integrated public health strategies aligned with the 2030 Agenda for Sustainable Development.
Epidemiological Analysis
Global Prevalence and Mortality
The scale of the Hepatitis B epidemic represents a major global health problem. Key statistics highlight the challenge:
- WHO estimates indicate that 254 million people were living with chronic Hepatitis B infection in 2022.
- The virus contributes to 1.2 million new infections annually.
- In 2022, Hepatitis B was responsible for an estimated 1.1 million deaths, primarily from cirrhosis and hepatocellular carcinoma.
The burden is disproportionately concentrated in the WHO Western Pacific and African Regions, which together account for over 160 million chronic infections. This regional disparity highlights inequities in health outcomes, a core concern of the SDG framework.
Modes of Transmission
Transmission dynamics are critical to understanding and interrupting the spread of the virus. The primary modes include:
- Perinatal Transmission: Mother-to-child transmission during birth is a common route in highly endemic areas. Infections in infancy and early childhood lead to chronic hepatitis in approximately 95% of cases, perpetuating the cycle of disease and challenging SDG 3.2 (end preventable deaths of newborns and children under 5).
- Exposure to Infected Bodily Fluids: The virus spreads through contact with blood or other body fluids via unsafe injections, exposure to sharp instruments, and sexual contact.
- Environmental Viability: The Hepatitis B virus can survive outside the body for at least seven days, posing an ongoing risk of infection for non-immune individuals.
Clinical Manifestations and Diagnosis
Symptomatology and Disease Progression
Many newly infected individuals are asymptomatic. When acute illness occurs, symptoms can include jaundice, dark urine, extreme fatigue, nausea, vomiting, and abdominal pain. While most adults recover from acute infection, a subset develops chronic Hepatitis B, which can progress to fatal complications such as cirrhosis and liver cancer. This progression directly impacts mortality rates related to non-communicable diseases (SDG Target 3.4).
Diagnostic Gaps and Linkage to Care
Effective diagnosis is essential for management and prevention, yet significant gaps persist, hindering progress toward Universal Health Coverage (UHC), a cornerstone of SDG 3 (Target 3.8). As of 2022, only 13% of individuals living with Hepatitis B were aware of their infection, and a mere 3% were receiving treatment. WHO recommends targeted testing for all pregnant women, blood donors, and high-risk populations to improve diagnosis rates and facilitate linkage to care and prevention services, including measures to prevent mother-to-child transmission.
Special Considerations: HBV-HIV Co-infection
Approximately 1% of persons with HBV (2.7 million people) are also infected with HIV. The co-epidemic complicates treatment and management, requiring integrated service delivery. WHO’s recommendation to treat all individuals diagnosed with HIV, using regimens that are also active against HBV, represents a synergistic approach that aligns with the SDG principle of leaving no one behind.
Strategic Interventions for SDG Attainment
Prevention through Vaccination
The availability of a safe and effective vaccine makes Hepatitis B a preventable disease. Vaccination is a cornerstone of the global strategy to eliminate the virus and is critical for achieving SDG 3 targets.
- Infant Vaccination: Universal administration of the Hepatitis B vaccine to all infants, starting with a birth dose within 24 hours, is the most effective intervention. A complete vaccine series offers nearly 100% protection for at least 20 years.
- Prevention of Mother-to-Child Transmission (PMTCT): Combining infant vaccination with antiviral therapy for eligible pregnant women can effectively prevent perinatal transmission.
- Safety Practices: Promoting safe sex, avoiding the sharing of needles, and ensuring sterile practices in healthcare and community settings are vital complementary prevention strategies.
The success of vaccination programs is evident in the drop in chronic HBV prevalence among children under five from approximately 5% in the pre-vaccine era to under 1% in 2019.
Treatment and Management
While there is no specific treatment for acute Hepatitis B, chronic infection can be managed with oral antiviral medications like tenofovir or entecavir. Treatment is a lifelong commitment for most patients but is crucial for:
- Slowing the progression of cirrhosis.
- Reducing the incidence of liver cancer.
- Improving long-term survival.
Expanding access to affordable treatment is essential for reducing premature mortality and achieving the goals of UHC (SDG Target 3.8).
Global Response and Strategic Framework
WHO’s Role in Achieving 2030 Targets
The World Health Organization (WHO) guides the global response through its Global Health Sector Strategies (GHSS) on HIV, viral hepatitis, and sexually transmitted infections for 2022–2030. These strategies are fully aligned with the 2030 Agenda for Sustainable Development and aim to end these epidemics as public health threats by 2030.
The GHSS framework promotes a synergistic approach under the umbrella of UHC and primary health care. It calls for countries to scale up prevention, testing, and treatment for viral hepatitis, with a focus on reaching the most affected communities and addressing health inequities. By developing evidence-based guidelines, supporting national strategies, and raising awareness through campaigns like World Hepatitis Day, WHO is driving global efforts to eliminate Hepatitis B and realize the vision of SDG 3 for a healthier future for all.
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
- The entire article focuses on Hepatitis B, a major global health problem that causes acute and chronic liver disease, cirrhosis, cancer, and death. It directly addresses the goal of ensuring healthy lives and promoting well-being for all at all ages by discussing disease prevalence, prevention (vaccines), diagnosis, and treatment. The article states, “Hepatitis B is a major global health problem,” and details its impact with “an estimated 1.1 million deaths” in 2022.
-
SDG 5: Gender Equality
- The article connects to this goal through its focus on mother-to-child transmission and the health of pregnant women. It highlights that the virus is “most commonly transmitted from mother to child during birth and delivery” and that prevention includes testing pregnant women. This addresses a key aspect of women’s health and reproductive rights.
-
SDG 10: Reduced Inequalities
- The article points to significant inequalities in the burden of Hepatitis B and access to care. It notes the highest burden is in the “WHO Western Pacific Region and the WHO African Region.” It also identifies specific high-risk and vulnerable populations that require targeted interventions, such as “migrants from endemic regions,” “people who inject drugs (PWID),” “people in prisons,” “men who have sex with men (MSM) sex workers,” and “transgender people.” The WHO response explicitly aims to address “gaps and inequities.”
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Target 3.3: End the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.
- This target is central to the article. The WHO’s strategy mentioned in the text has the explicit goal of “ending AIDS, viral hepatitis (especially chronic hepatitis B and C) and sexually transmitted infections by 2030.” The article also discusses “HBV-HIV coinfection,” directly linking the fight against hepatitis to the fight against AIDS.
-
Target 3.4: By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment…
- The article links the communicable disease of Hepatitis B directly to non-communicable diseases (NCDs). It states that Hepatitis B results in deaths “mostly from cirrhosis and hepatocellular carcinoma (primary liver cancer).” By preventing and treating Hepatitis B, the mortality from these NCDs is reduced.
-
Target 3.8: Achieve universal health coverage (UHC), including… access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
- The article emphasizes the need for universal access to Hepatitis B services. It mentions that the WHO strategy promotes “synergies under a universal health coverage and primary health care framework.” The low diagnosis rate (“13%… were aware of their infection”) and treatment rate (“3%… were on treatment”) highlight the significant gap in achieving UHC for this disease. The availability of a “safe, available and effective” vaccine is a core component of this target.
-
Target 3.b: Support the research and development of vaccines and medicines for the communicable and non-communicable diseases that primarily affect developing countries…
- The article underscores the success and importance of the Hepatitis B vaccine, a key outcome of R&D. It states, “Hepatitis B can be prevented by vaccines that are safe, available and effective.” The discussion of antiviral treatments like “tenofovir or entecavir” and updated WHO guidelines also falls under this target. The regional burden data shows the disease primarily affects developing countries.
-
Target 5.6: Ensure universal access to sexual and reproductive health and reproductive rights…
- The article’s focus on preventing mother-to-child transmission directly relates to this target. The recommendation that WHO “recommends testing… of all pregnant women” is a key intervention within sexual and reproductive healthcare services to protect both mother and child.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
For Target 3.3 (Combat Hepatitis):
- Hepatitis B Incidence: The article states there are “1.2 million new infections each year.” Tracking this number measures progress.
- Hepatitis B Prevalence: The article notes “254 million people were living with chronic hepatitis B infection in 2022.” A reduction in this number would indicate progress. A key success metric is also provided: “the proportion of children under five years of age chronically infected with HBV dropped to just under 1% in 2019 down from around 5% in the pre-vaccine era.”
- Hepatitis B Mortality Rate: The article provides a baseline: “In 2022, hepatitis B resulted in an estimated 1.1 million deaths.” Reducing this number is a direct measure of success.
-
For Target 3.8 (Universal Health Coverage):
- Diagnosis Coverage: The article explicitly states a key indicator: “As of 2022, 13% of all people estimated to be living with hepatitis B were aware of their infection.” Increasing this percentage is a measure of progress.
- Treatment Coverage: A clear indicator is provided: “3% (7 million) of the people living with chronic hepatitis B were on treatment.” Increasing this percentage is a critical metric.
- Vaccination Coverage: While not giving a global percentage, the article implies this is a key indicator by stating, “All babies should receive the hepatitis B vaccine as soon as possible after birth,” and by noting the successful drop in childhood infection rates due to the vaccine.
-
For Target 5.6 (Sexual and Reproductive Health):
- (Implied) Testing Rate in Pregnant Women: The article states that WHO “recommends testing… of all pregnant women.” This implies that the proportion of pregnant women who are tested for Hepatitis B is a key performance indicator for preventing mother-to-child transmission.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators (Mentioned or Implied in the Article) |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.3: End epidemics… and combat hepatitis… |
|
| 3.4: Reduce premature mortality from non-communicable diseases… |
|
|
| 3.8: Achieve universal health coverage… |
|
|
| 3.b: Support R&D of vaccines and medicines… |
|
|
| SDG 5: Gender Equality | 5.6: Ensure universal access to sexual and reproductive health… |
|
| SDG 10: Reduced Inequalities | 10.2: Promote the inclusion of all… |
|
Source: who.int
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0