Looming Medicaid work requirements could worsen Missouri backlogs in social services – KSMU

Proposed Medicaid Work Requirements and Implications for Sustainable Development Goals
Introduction: Policy Overview and SDG Context
A new federal budget proposal introduces mandatory work requirements for Medicaid recipients aged 19 to 64, scheduled for implementation in December 2026. This policy mandates that enrollees document 80 hours of work, education, caregiving, or volunteering per month to maintain eligibility. This report analyzes the potential impacts of these requirements in Missouri, with a significant focus on their alignment with the United Nations Sustainable Development Goals (SDGs), particularly SDG 1 (No Poverty), SDG 3 (Good Health and Well-being), SDG 8 (Decent Work and Economic Growth), SDG 10 (Reduced Inequalities), and SDG 16 (Peace, Justice, and Strong Institutions).
Direct Impacts on Health, Poverty, and Well-being (SDG 3 & SDG 1)
The proposed requirements are projected to have a severe negative impact on public health and poverty reduction efforts, directly contravening the objectives of SDG 3 and SDG 1.
Projected Loss of Coverage and Financial Hardship
- Nationally, an estimated 10 million Americans are projected to become uninsured.
- In Missouri, approximately 130,000 individuals are at risk of losing their Medicaid coverage.
- Federal Medicaid spending is estimated to decrease by $911 billion over ten years, with $326 billion in savings attributed to the work requirements.
Evidence from a similar program implemented in Arkansas demonstrates the direct consequences of coverage loss, which undermines both health and financial stability:
- Increased Medical Debt: 50% of those who lost coverage reported serious problems paying off medical debt, pushing them closer to or into poverty (violating SDG 1).
- Delayed Medical Care: 56% delayed necessary medical care due to cost (violating SDG 3).
- Delayed Medication: 64% delayed filling prescriptions due to cost (violating SDG 3).
Institutional and Economic Challenges (SDG 16 & SDG 8)
The policy presents significant administrative and economic challenges that threaten the efficacy of public institutions and sustainable economic growth, impacting SDG 16 and SDG 8.
Strain on State Administrative Systems
Missouri’s social services infrastructure is already under pressure, with a history of failing to meet the federally mandated 45-day processing time for Medicaid applications. The new policy would intensify this institutional strain by:
- Requiring a new, complex system to verify work, volunteering, or caregiving hours.
- Doubling the workload for eligibility verification by shifting from annual to semi-annual checks.
- Increasing confusion for enrollees navigating multi-page notifications and complex documentation requirements, further burdening state resources.
Economic Inefficiency and Employment Outcomes
The policy’s premise of promoting employment is not supported by evidence, while its administrative costs are substantial, challenging the principles of SDG 8.
- High Administrative Costs: Arkansas spent over $26 million on administrative and implementation costs for its short-lived program.
- Minimal Impact on Employment: Studies show the requirements did not significantly increase employment. Over 95% of the target group in Arkansas were already working or qualified for an exemption.
- Existing Workforce Participation: KFF data from 2023 shows that the vast majority of adult Medicaid recipients are already engaged in activities that would meet the requirements, with only 8% not working for other reasons.
- 44% work full-time.
- 20% work part-time.
- 12% are caregivers.
- 10% have an illness or disability.
- 7% are in school.
Exacerbating Inequalities in Rural Communities (SDG 10)
The work requirements are poised to disproportionately harm rural populations, deepening inequalities and undermining the core principle of SDG 10, “leave no one behind.”
Barriers to Compliance and Access
Rural residents face unique hurdles in meeting and documenting the requirements:
- Digital Divide: Lack of reliable internet access and technology, such as smartphones, makes online reporting burdensome or impossible.
- Transportation and Job Access: Limited transportation options and a scarcity of jobs offering consistent hours create significant barriers to meeting the 80-hour monthly threshold.
- Economic Vulnerability: Workers in retail and service industries with fluctuating shifts are at high risk of losing coverage despite being employed.
Threat to Rural Health Infrastructure
The loss of Medicaid revenue could destabilize the rural healthcare system, which is critical for community well-being and local economies (SDG 3, SDG 8).
- Rural hospitals are heavily dependent on Medicaid reimbursements to remain operational.
- Recent data indicates that 44% of rural hospitals already operate with negative financial margins.
- The closure of a local hospital or clinic due to funding cuts would devastate the local economy and eliminate access to essential health services, creating a “perfect storm” of negative consequences for working families in these communities.
1. Which SDGs are addressed or connected to the issues highlighted in the article?
The article on changes to Missouri’s Medicaid program touches upon several Sustainable Development Goals (SDGs) due to its focus on health care access, poverty, inequality, and the administrative capacity of public institutions.
-
SDG 1: No Poverty
The article connects to this goal because Medicaid is a social safety net program for low-income individuals. The potential loss of health coverage can lead to increased medical debt and financial instability, pushing people into or deeper into poverty. The article notes that in Arkansas, after similar requirements were implemented, “half of those who had lost Medicaid… reported serious problems paying off medical debt.”
-
SDG 3: Good Health and Well-being
This is the most central SDG in the article. The entire discussion revolves around access to health insurance (Medicaid), which is fundamental to ensuring healthy lives. The proposed work requirements threaten to increase the number of uninsured people (“increase the number of uninsured Americans by 10 million”), which directly impacts public health outcomes. The article cites that 56% of those who lost coverage in Arkansas “delayed some form of medical care due to the cost and 64% delayed medication due to the cost.”
-
SDG 8: Decent Work and Economic Growth
The policy change introduces work requirements as a condition for receiving health benefits. However, the article questions the effectiveness of this policy in promoting employment, citing a study that found the requirements in Arkansas “did little to increase the number of enrollees who were employed.” It also highlights the precarious nature of work for many enrollees (e.g., retail workers, cooks) whose fluctuating hours could put them at risk of losing coverage despite being employed.
-
SDG 10: Reduced Inequalities
The article highlights how the new rules could exacerbate inequalities, particularly for vulnerable populations. It points out the specific challenges faced by people in rural Missouri, such as “unreliable internet or technology access” and lack of transportation, which create additional hurdles to meeting the reporting requirements. This creates an unequal system where location and socioeconomic status determine access to essential services.
-
SDG 16: Peace, Justice and Strong Institutions
This goal is relevant because the article extensively discusses the capacity and effectiveness of state institutions. It notes that “For years, Missouri has struggled to process social services applications in a timely manner” and that the new rules will add a significant administrative burden on an “outdated system that is struggling.” The ability of the state agency to implement the new policy effectively, transparently, and accountably is a core theme.
2. What specific targets under those SDGs can be identified based on the article’s content?
Based on the issues discussed, several specific SDG targets can be identified:
-
Target 1.3: Implement nationally appropriate social protection systems and measures for all.
The article is centered on Medicaid, which is a key social protection system in the United States. The discussion about expanding or restricting eligibility through work requirements directly relates to the implementation and coverage of this system for “the poor and the vulnerable.” The potential for “130,000 people losing access to Medicaid” in Missouri is a direct challenge to this target.
-
Target 3.8: Achieve universal health coverage, including financial risk protection and access to quality essential health-care services.
This target is directly addressed. The article focuses on the potential loss of health coverage, which moves away from the goal of universal coverage. It also highlights the lack of financial risk protection when people lose insurance, citing the “serious problems paying off medical debt” experienced by those who lost coverage in Arkansas. The delay of medical care and medication due to cost further illustrates a failure to provide access to essential health-care services.
-
Target 10.4: Adopt policies, especially fiscal, wage and social protection policies, and progressively achieve greater equality.
The article analyzes a change in social protection policy (the new Medicaid rules) and its potential to increase, rather than reduce, inequality. The disproportionate impact on rural residents who “may not even have a smartphone and definitely not internet access” shows how the policy could fail to achieve greater equality.
-
Target 16.6: Develop effective, accountable and transparent institutions at all levels.
The article questions the effectiveness of the state agency responsible for Medicaid. It points to Missouri’s history of failing to meet federal deadlines for processing applications (“repeatedly violated the time frame requirements”) and the concern that the new, more complex rules will overwhelm an already “struggling” system. The discussion about the high administrative costs (“$26 million in administrative costs” in Arkansas) also relates to institutional efficiency.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
Yes, the article mentions or implies several quantitative and qualitative indicators that can be used to measure progress.
-
Indicator for Target 1.3 & 3.8: Number/Proportion of population covered by health insurance.
The article provides specific numbers that serve as direct indicators. It states the new rules could “increase the number of uninsured Americans by 10 million” and cause “an estimated 130,000 people losing access to Medicaid” in Missouri. Tracking these numbers would measure progress (or regression) toward social protection and universal health coverage.
-
Indicator for Target 3.8: Proportion of population facing catastrophic health expenditure.
This is implied through the mention of medical debt. The finding that “half of those in Arkansas who had lost Medicaid as part of the requirements reported serious problems paying off medical debt” serves as a proxy indicator for financial hardship due to health care costs.
-
Indicator for Target 8.5: Employment rate of the target population.
The article provides baseline data: “In 2023, 44% of the adults 19-64 enrolled in Medicaid were working full time, while 20% were working part time.” It also notes that a study in Arkansas found “no significant upticks in employment as a result of the requirements.” This allows for measuring whether the policy actually achieves its stated goal of increasing work.
-
Indicator for Target 16.6: Timeliness of administrative processes.
A clear indicator is mentioned: the 45-day federal requirement for processing Medicaid applications. The article states that “Missouri has repeatedly violated the time frame requirements,” making this a measurable indicator of institutional performance.
-
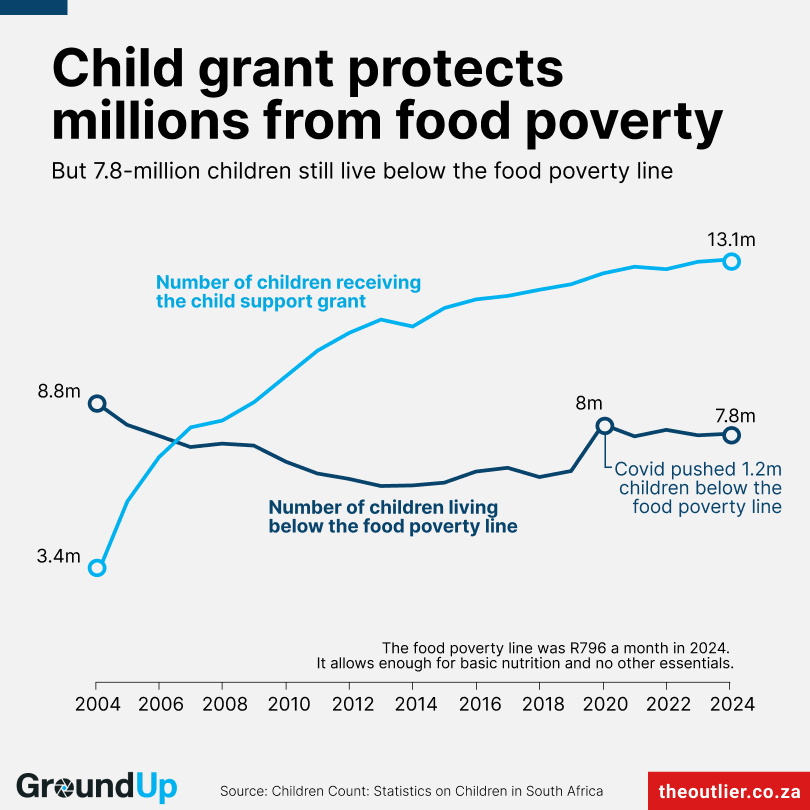
Indicator for Target 10.4 & 3.8: Disparities in health coverage and outcomes by geographic location (rural vs. urban).
This is implied by the discussion of challenges in rural Missouri. An indicator would be the rate of coverage loss in rural versus urban areas. Furthermore, the article mentions that “44% of rural hospitals have negative margins” and that closures could result from Medicaid cuts, indicating a widening health infrastructure gap between rural and urban communities.
4. Create a table with three columns titled ‘SDGs, Targets and Indicators” to present the findings from analyzing the article.
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 1: No Poverty | 1.3: Implement nationally appropriate social protection systems and measures for all. |
|
| SDG 3: Good Health and Well-being | 3.8: Achieve universal health coverage, including financial risk protection and access to quality essential health-care services. |
|
| SDG 8: Decent Work and Economic Growth | 8.5: Achieve full and productive employment and decent work for all. |
|
| SDG 10: Reduced Inequalities | 10.4: Adopt policies, especially… social protection policies, and progressively achieve greater equality. |
|
| SDG 16: Peace, Justice and Strong Institutions | 16.6: Develop effective, accountable and transparent institutions at all levels. |
|
Source: ksmu.org

What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0