macrophages via oxLDL-mediated metabolic interplay in hepatocellular carcinoma – Nature
Report on a Novel Therapeutic Avenue for Hepatocellular Carcinoma and its Contribution to Sustainable Development Goal 3
This report details findings from a study investigating the cellular and metabolic mechanisms underlying Hepatocellular Carcinoma (HCC) progression and immunotherapy resistance. The research identifies a novel therapeutic axis that directly supports the United Nations Sustainable Development Goal 3 (Good Health and Well-being), particularly Target 3.4, which aims to reduce premature mortality from non-communicable diseases like cancer.
Introduction and Context
The Global Burden of Hepatocellular Carcinoma (HCC)
Hepatocellular Carcinoma (HCC) represents a significant global health challenge and is the fourth leading cause of cancer-related death worldwide. The high mortality rate associated with HCC directly impedes progress toward SDG Target 3.4. A primary obstacle to effective treatment is the profound intratumoral heterogeneity (ITH), which drives metastasis, recurrence, and therapeutic resistance. This study sought to deconstruct this heterogeneity to identify actionable therapeutic targets.
Research Objectives
The primary objective was to create a comprehensive single-cell atlas of HCC to understand the functional programs of cancer cells and their impact on the tumor microenvironment (TME). By elucidating these interactions, the research aimed to uncover novel mechanisms of immune suppression and identify therapeutic strategies to improve patient outcomes, aligning with SDG Target 3.b (support for research and development of new medicines).
Key Research Findings
Identification of Three Functional Cancer Cell Archetypes
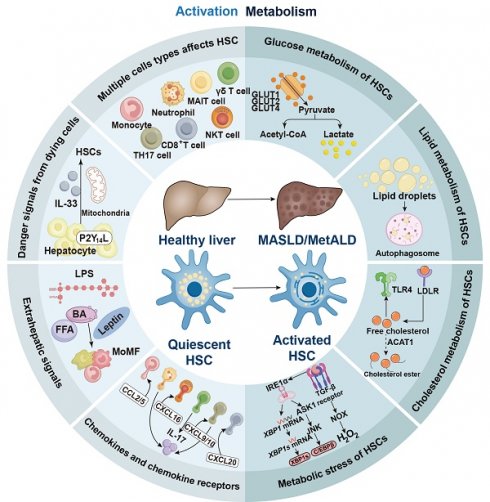
Through single-nucleus and single-cell RNA sequencing, the study identified three distinct and co-existing functional archetypes within HCC cancer cells, each with a unique spatial distribution within the tumor:
- Metabolism Archetype: Characterized by enhanced lipid, lipoprotein, and cholesterol metabolism.
- Stemness Archetype: Exhibiting signatures of protein translation, epithelial-to-mesenchymal transition (EMT), and cancer stem cells.
- Inflammation Archetype: Defined by acute-phase and complement system responses.
An Immuno-Inhibitory Niche Linked to Poor Prognosis
A critical finding was the identification of an immuno-inhibitory niche that compromises patient outcomes and response to immunotherapy. This niche is characterized by:
- The spatial co-localization of metabolism archetype cancer cells and a specific population of tumor-associated macrophages (TREM2+ TAMs).
- The exclusion of effector immune cells, such as CD8+ T cells, from this niche.
- A strong association between the presence of this niche and inferior patient survival and resistance to anti-PD1 immunotherapy.
Mechanistic Insights into Tumor Progression
The oxLDL-Mediated Metabolic Interplay
The study elucidated the precise mechanism driving the formation of this immunosuppressive niche. The process occurs in a sequential manner:
- Metabolism archetype cancer cells exhibit upregulated expression of squalene epoxidase (SQLE), a rate-limiting enzyme in cholesterol biosynthesis.
- The increased SQLE activity facilitates the generation and accumulation of oxidized LDL (oxLDL) within the tumor microenvironment.
- oxLDL acts as a signaling molecule that induces the polarization and recruitment of TREM2+ TAMs via the TREM2-SYK-CEBPα signaling axis in macrophages.
Pro-Tumorigenic Actions of TREM2+ TAMs
Once polarized by oxLDL, TREM2+ TAMs actively promote cancer progression and immunotherapy resistance through a dual-action mechanism mediated by the secretion of SPP1 (Osteopontin):
- Action on Cancer Cells: SPP1 signaling promotes cancer cell invasion and confers resistance to apoptosis induced by effector cytokines (TNF and IFNγ).
- Action on T Cells: SPP1 signaling directly impairs the function of CD8+ T cells, contributing to an exhausted and ineffective anti-tumor immune response.
Implications for Sustainable Development Goals (SDGs)
Advancing SDG Target 3.4: Reducing Mortality from Non-Communicable Diseases
By identifying the SQLE-oxLDL-TREM2 axis as a key driver of HCC progression and immunotherapy failure, this research provides a clear strategy to improve treatment efficacy. Targeting this pathway can disrupt the immunosuppressive TME, making tumors more susceptible to immunotherapy and potentially reducing premature mortality from HCC, a major NCD.
Supporting SDG Target 3.b: Research and Development of New Medicines
The study successfully identifies and validates two distinct therapeutic targets:
- Cancer Cell-Intrinsic SQLE: An enzyme within the tumor cells that initiates the immunosuppressive cascade.
- Macrophage-Specific TREM2: A receptor on immune cells that responds to the tumor’s metabolic signals.
This provides a strong foundation for the development of new drugs or combination therapies aimed at these targets.
A Promising Therapeutic Avenue for Enhanced and Accessible Immunotherapy
The research demonstrates that inhibiting the identified pathway can restore anti-tumor immunity. Significantly, experiments in mouse models showed that combining an FDA-approved SQLE inhibitor (terbinafine) with anti-PD1 therapy synergistically suppressed tumor growth. This finding has profound implications for SDG Target 3.8 (Achieve universal health coverage and access to affordable essential medicines), as repurposing an existing, affordable drug could provide a cost-effective strategy to enhance the efficacy of expensive immunotherapies for a broad patient population.
Conclusion
This study reveals a critical metabolic interplay between metabolism-focused cancer cells and TREM2+ macrophages, driven by oxLDL, which establishes an immunosuppressive niche and fosters immunotherapy resistance in HCC. The identification of the SQLE-oxLDL-TREM2 axis offers a promising and actionable therapeutic strategy. Targeting this pathway, potentially with existing drugs like terbinafine, could significantly improve clinical outcomes for HCC patients, thereby making a substantial contribution to the global public health objectives outlined in SDG 3.
SDGs Addressed in the Article
-
SDG 3: Good Health and Well-being
- The article’s central theme is the study of Hepatocellular Carcinoma (HCC), a significant global health problem. It directly addresses the goal of ensuring healthy lives by investigating a disease that is the “fourth leading cause of cancer-related death worldwide.” The research aims to understand the complex mechanisms of HCC to develop more effective treatments, which is fundamental to improving health outcomes and promoting well-being.
Specific Targets Identified
-
Target 3.4: Reduce premature mortality from non-communicable diseases
- Explanation: The article explicitly highlights the high mortality associated with HCC, stating it has a “dismal 5-year survival rate below 20%.” The entire study is geared towards finding new therapeutic strategies (“offering a promising therapeutic avenue for HCC immunotherapies”) to improve patient outcomes, directly contributing to the goal of reducing premature deaths from non-communicable diseases like cancer.
-
Target 3.b: Support research and development of medicines for non-communicable diseases
- Explanation: The research presented is a clear example of efforts under this target. The study uses advanced techniques like “single-nucleus RNA sequencing (snRNA-seq), scRNA-seq, and spatial transcriptomic sequencing” to understand disease mechanisms. Furthermore, it identifies and tests potential therapeutic targets, such as the SQLE enzyme, and even evaluates an existing FDA-approved drug, terbinafine, for its potential to “enhance immunotherapy efficacy in HCC.” This directly supports the research and development of new medicines.
Indicators for Measuring Progress
-
Indicator 3.4.1: Mortality rate attributed to cancer
- Explanation: The article provides direct context for this indicator by stating that HCC is the “fourth leading cause of cancer-related death worldwide.” It also mentions that the majority of patients have a “dismal 5-year survival rate below 20%,” which is a key metric related to cancer mortality. The research aims to improve these statistics, making the mortality rate a relevant measure of progress.
-
Indicator 3.b.1: Proportion of the population with access to affordable medicines
- Explanation: While not directly measuring access, the article’s research is a crucial prerequisite for developing new and potentially more affordable treatments. The investigation into “an FDP-approved SQLE inhibitor, terbinafine,” suggests that repurposing existing, approved drugs could be a pathway to creating more accessible therapeutic options. The study’s goal to “offer a promising therapeutic avenue for HCC immunotherapies” implies a focus on developing treatments that can eventually be made available to patients, thus relating to the core aim of this indicator.
Summary Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.4: By 2030, reduce by one-third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being. | 3.4.1: Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease. The article notes HCC is the “fourth leading cause of cancer-related death worldwide” with a “dismal 5-year survival rate below 20%.” |
| SDG 3: Good Health and Well-being | 3.b: Support the research and development of vaccines and medicines for the communicable and non-communicable diseases that primarily affect developing countries, provide access to affordable essential medicines and vaccines. | 3.b.1: Proportion of the population with access to affordable medicines and vaccines on a sustainable basis. The research aims to find “a promising therapeutic avenue for HCC immunotherapies” and tests an existing approved drug (terbinafine), which are foundational steps for developing accessible medicines. |
Source: nature.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0