Nutritional status, body composition and chemotherapy dosing in children and young people with cancer: a systematic review by the SIOP nutrition network – Nature
Report on Nutritional Status, Body Composition, and Chemotherapy Dosing in Children and Young People with Cancer
Abstract
Malnutrition, including undernutrition and overweight/obesity, significantly affects the pharmacokinetics and pharmacodynamics of antineoplastic drugs in children and adolescents under 21 years. A systematic review of literature up to September 30, 2024, identified 18 relevant studies examining pharmacokinetic parameters for drugs such as mercaptopurine, vincristine, anthracyclines, methotrexate, busulfan, bevacizumab, and crizotinib. Due to study heterogeneity and limited data, no dosing recommendations were established. The rising burden of childhood cancer in low-to-middle-income countries (LMIC), coupled with high undernutrition and obesity prevalence, underscores the urgent need for standardized research to optimize treatment globally, aligning with Sustainable Development Goals (SDGs) 3 (Good Health and Well-being) and 2 (Zero Hunger).
Background
Childhood cancer survival rates exceed 80% in high-income countries (HIC) due to advanced treatment protocols involving intensive chemotherapy. However, these protocols increase toxicity and long-term chronic disease risk, affecting survivors’ quality of life. Approximately 90% of global childhood cancer cases occur in LMIC, where undernutrition is prevalent, and obesity rates are rising globally, impacting treatment outcomes. Nutritional status, encompassing weight, height, body composition, and dietary intake, influences drug disposition and clinical outcomes. Malnutrition is a modifiable prognostic risk factor, affecting survival and toxicity in pediatric oncology. Understanding the impact of nutritional status on drug pharmacokinetics and pharmacodynamics is critical for optimizing pediatric cancer care, supporting SDG 3.
Methods
Systematic Literature Review
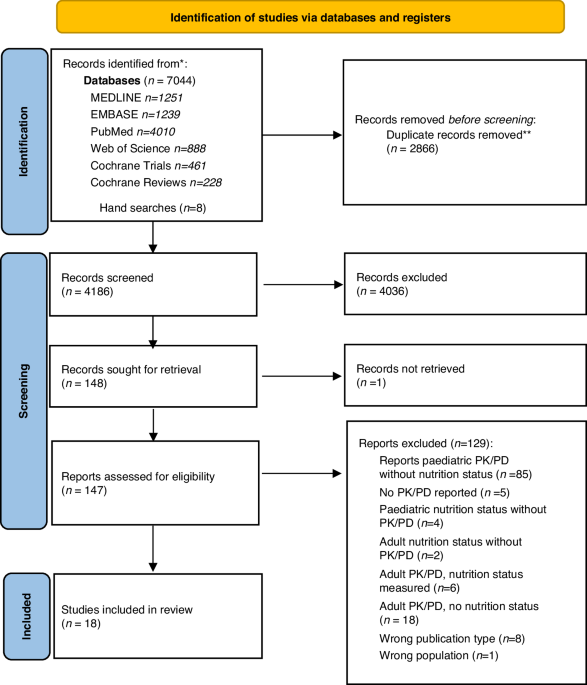
The International Society of Paediatric Oncology (SIOP) Nutrition Network conducted a systematic literature review following PRISMA guidelines and registered in PROSPERO (CRD42023435261). Multiple databases were searched for studies involving children under 21 years with cancer receiving chemotherapy, assessing pharmacokinetic and pharmacodynamic parameters relative to nutritional status. Inclusion criteria encompassed all study designs without language or date restrictions. Screening and data extraction were performed independently by reviewers, with quality assessed using GRADE and risk of bias tools.
Study Selection and Data Extraction
- 4186 articles screened
- 150 full texts reviewed
- 18 studies included for data extraction
Results
Study Characteristics
- 18 studies included, with 1194 children aged under 21 years
- Most studies prospective; drugs studied include anthracyclines (doxorubicin, daunorubicin), methotrexate, busulfan, vincristine, mercaptopurine, bevacizumab, crizotinib
- Pharmacokinetic parameters assessed mainly drug clearance and volume of distribution
- Definitions of nutritional status varied; BMI commonly used, with some studies using body composition measures
Impact of Nutritional Status on Pharmacokinetics
Undernutrition
- Undernutrition associated with altered drug clearance and increased drug exposure for vincristine, methotrexate, and doxorubicin in some studies
- Children with extreme undernutrition required higher busulfan doses to achieve target drug exposure
- Variability in defining undernutrition and lack of data on severe malnutrition limit conclusions
Overweight and Obesity
- Obesity influenced pharmacokinetics variably; some studies reported altered clearance and volume of distribution for drugs such as mercaptopurine, methotrexate, doxorubicin, busulfan, and crizotinib
- Obese children showed increased risk of delayed methotrexate elimination and altered drug exposure
- Dosing strategies varied, with some evidence supporting dosing based on actual body weight to avoid underdosing
- Standardized obesity classification and body composition assessment are needed
Outcomes
- Malnutrition (both undernutrition and obesity) linked to increased toxicity, decreased survival, and relapse risk in pediatric cancer
- Some studies reported increased cardiotoxicity with doxorubicin in undernourished children
- Data on pharmacokinetics linked to clinical outcomes remain limited
Pharmacogenetics
- Genetic polymorphisms influence antineoplastic drug pharmacokinetics, particularly for anthracyclines
- Integration of pharmacogenetics with nutritional status is essential for personalized dosing
- Most pharmacogenetic data derive from Caucasian populations; diverse ethnic representation is needed
Study Quality
The overall quality of evidence was very low due to heterogeneity, small sample sizes, and inconsistent methodologies.
Discussion
Drug Dosing Considerations
- Body surface area (BSA) is commonly used for chemotherapy dosing but may inadequately reflect altered body composition in malnourished or obese children
- Drug lipophilicity affects distribution and dosing requirements, especially in obesity
- Standardized nutritional assessment using BMI, mid-upper arm circumference (MUAC), and body composition measures is recommended
- Future research should incorporate uniform definitions, pharmacogenetics, and diverse populations to optimize dosing
Effect of Nutritional Status on Pharmacokinetics
Undernutrition
- Evidence indicates altered pharmacokinetics in undernourished children, but data are limited and inconsistent
- Severe malnutrition common in LMIC is underrepresented in studies
- Micronutrient deficiencies and their impact on drug metabolism require further investigation
Overweight and Obesity
- Obesity may alter drug clearance and distribution, affecting efficacy and toxicity
- Standardized obesity classification and consideration of body fat percentage are critical
- Sex-based differences and genetic factors need exploration
Nutritional Status and Clinical Outcomes
- Malnutrition is associated with poorer treatment outcomes, including survival and toxicity
- Data linking pharmacokinetics, nutritional status, and outcomes are sparse
- Enhanced pharmacokinetic monitoring and outcome reporting are essential
Recommendations and Conclusion
- There is a critical need for standardized nutritional assessment and pharmacokinetic evaluation in pediatric oncology, especially in LMIC
- Use of international cutoffs for undernutrition and obesity, and incorporation of body composition measures, is recommended
- Prospective studies should integrate pharmacogenetics, ethnicity, and standardized dosing strategies
- Regular monitoring of chemotherapy drug levels is advised for children with altered nutritional status
- These efforts align with SDG 3 (Good Health and Well-being) and SDG 10 (Reduced Inequalities) by improving equitable cancer care globally
Funding and Acknowledgements
This work was supported by the International Society of Paediatric Oncology (SIOP). The authors acknowledge assistance in search strategy development from the University of Auckland.
1. Sustainable Development Goals (SDGs) Addressed or Connected
- SDG 3: Good Health and Well-being
- The article focuses on childhood cancer treatment outcomes, pharmacokinetics, and pharmacodynamics of antineoplastic drugs, which are directly related to ensuring healthy lives and promoting well-being for all ages.
- It addresses issues of malnutrition (undernutrition and obesity) affecting treatment efficacy and toxicity, impacting survival and quality of life of children with cancer.
- It highlights the need for optimized treatment protocols and dosing strategies to improve health outcomes globally, especially in low-to-middle-income countries (LMIC).
- SDG 2: Zero Hunger
- The article discusses malnutrition, including undernutrition and overweight/obesity, which relates to ending all forms of malnutrition and ensuring access to nutritious food.
- It emphasizes the high prevalence of undernutrition in LMIC and the global burden of childhood obesity, linking nutritional status to cancer treatment outcomes.
- SDG 10: Reduced Inequalities
- The article highlights disparities in childhood cancer burden and nutritional status between high-income countries (HIC) and LMIC.
- It calls for more research and standardized approaches that include diverse ethnic representation and address global inequities in pediatric cancer care.
2. Specific Targets Under Identified SDGs
- SDG 3: Good Health and Well-being
- Target 3.2: End preventable deaths of newborns and children under 5 years of age, aiming to reduce mortality from diseases including cancer.
- Target 3.8: Achieve universal health coverage, including access to quality essential health-care services and access to safe, effective, quality, and affordable essential medicines and vaccines.
- Target 3.b: Support the research and development of vaccines and medicines for communicable and non-communicable diseases that primarily affect developing countries.
- SDG 2: Zero Hunger
- Target 2.2: End all forms of malnutrition, including achieving targets on stunted and wasted children under 5 years of age and address the nutritional needs of adolescent girls, pregnant and lactating women, and older persons.
- SDG 10: Reduced Inequalities
- Target 10.2: Empower and promote the social, economic and political inclusion of all, irrespective of age, sex, disability, race, ethnicity, origin, religion or economic or other status.
- Target 10.3: Ensure equal opportunity and reduce inequalities of outcome, including by eliminating discriminatory laws, policies and practices.
3. Indicators Mentioned or Implied to Measure Progress
- Health and Treatment Outcomes Indicators
- Overall survival rates and event-free survival rates in children with cancer.
- Treatment-related toxicity and adverse events incidence.
- Pharmacokinetic parameters such as drug clearance, volume of distribution, area under the plasma concentration-time curve (AUC), and peak plasma concentrations.
- Incidence of treatment-related cardiotoxicity and neurotoxicity.
- Nutritional Status Indicators
- Body Mass Index (BMI) percentiles and z-scores for age.
- Prevalence of undernutrition (e.g., BMI-for-age ≤5th or 10th percentile) and obesity (BMI-for-age ≥95th percentile).
- Body composition measures such as percentage body fat via dual energy x-ray absorptiometry (DXA).
- Use of standardized international cutoffs for malnutrition and obesity (e.g., WHO and CDC growth charts).
- Pharmacogenetic Indicators
- Presence of single nucleotide polymorphisms (SNPs) affecting drug metabolism enzymes (e.g., FMO3, GSTP1, CYP3A5).
- Research and Monitoring Indicators
- Number and quality of prospective studies incorporating standardized nutritional assessment and pharmacokinetic analyses.
- Regular monitoring of chemotherapy blood/plasma concentrations in pediatric cancer patients with altered nutritional status.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being |
|
|
| SDG 2: Zero Hunger |
|
|
| SDG 10: Reduced Inequalities |
|
|
Source: nature.com








