Study examines decline of obstetric services in rural and urban hospitals – American Hospital Association
Report on the Decline of Obstetric Services and Implications for Sustainable Development Goals
1.0 Introduction
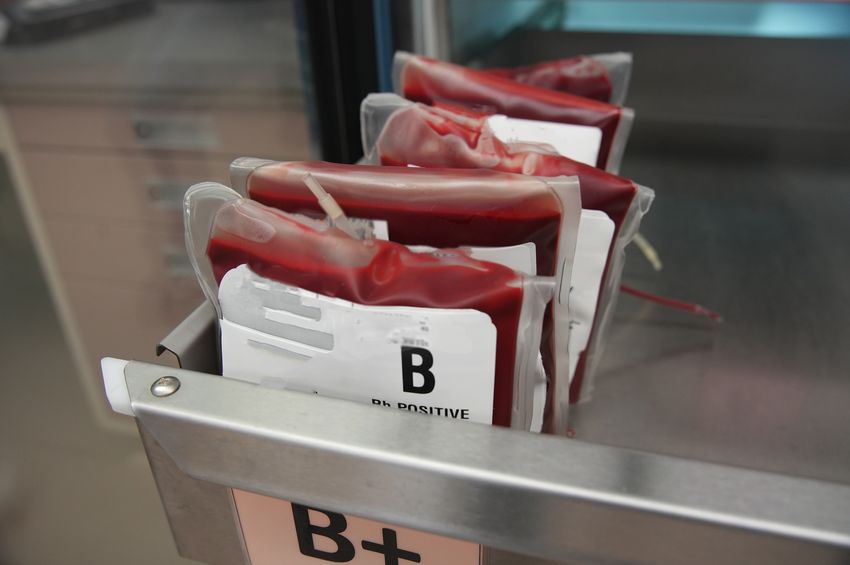
A recent analysis of hospital data from 2010 to 2022 reveals a significant decline in the provision of obstetric services across the United States. This trend, documented in a Health Affairs study using American Hospital Association (AHA) and Centers for Medicare & Medicaid Services (CMS) data, presents substantial challenges to the achievement of key United Nations Sustainable Development Goals (SDGs), particularly those related to health, equality, and sustainable communities.
2.0 Key Findings: A Nationwide Reduction in Obstetric Care
The study highlights a critical reduction in access to maternal healthcare, with pronounced effects in rural areas. These findings directly impact the framework for global sustainable development.
- State-Level Service Loss: Seven states witnessed a reduction of obstetric services in at least 25% of their total hospitals between 2010 and 2022.
- Urban Service Decline: By 2022, five states reported that 25% or more of their urban hospitals had ceased providing obstetric care.
- Rural Service Crisis: The decline was more acute in rural regions.
- Twelve states experienced a loss of obstetric services in 25% or more of their rural hospitals.
- By 2022, more than two-thirds of rural hospitals in eight separate states were operating without any obstetric services.
3.0 Analysis of Impact on Sustainable Development Goals (SDGs)
The erosion of obstetric care infrastructure has direct and adverse consequences for several SDGs.
3.1 SDG 3: Good Health and Well-being
- The closure of obstetric units is a direct impediment to achieving Target 3.1, which aims to reduce the global maternal mortality ratio.
- Reduced local access to care compromises Target 3.2, focused on ending preventable deaths of newborns and children, as it increases risks associated with childbirth and immediate postnatal care.
3.2 SDG 10: Reduced Inequalities
- The data reveals a severe disparity in healthcare access between rural and urban populations, undermining the objective of Target 10.2 to promote universal social inclusion and reduce inequalities in outcomes.
- The creation of “maternity care deserts,” especially in rural areas, exacerbates geographic and socio-economic inequalities, denying equitable access to essential health services for women and children.
3.3 SDG 5: Gender Equality
- The decline in available services directly challenges Target 5.6, which calls for universal access to sexual and reproductive health and reproductive rights.
- Ensuring access to safe and reliable maternal healthcare is a cornerstone of gender equality, and the reduction of these services disproportionately affects women, limiting their health, well-being, and economic stability.
1. Which SDGs are addressed or connected to the issues highlighted in the article?
SDG 3: Good Health and Well-being
- The article’s central theme is the “decline of obstetric services in rural and urban hospitals,” which directly pertains to the provision of health care and the well-being of mothers and newborns. This aligns with the goal of ensuring healthy lives and promoting well-being for all at all ages.
SDG 10: Reduced Inequalities
- The article explicitly highlights a disparity in healthcare access based on geographic location. It states that the loss of obstetric services was “more pronounced in rural areas,” pointing to an inequality between rural and urban populations in their ability to access essential maternal health care.
SDG 5: Gender Equality
- Obstetric services are a critical component of women’s health care. The reduction in access to these services disproportionately affects women, impacting their health, safety, and reproductive rights. Ensuring access to maternal care is fundamental to achieving gender equality.
2. What specific targets under those SDGs can be identified based on the article’s content?
SDG 3: Good Health and Well-being
- Target 3.1: By 2030, reduce the global maternal mortality ratio to less than 70 per 100,000 live births. The article’s focus on the decline in obstetric services is directly relevant, as a lack of access to skilled care during pregnancy and childbirth is a primary driver of maternal mortality. The closure of these services creates “maternity care deserts,” which poses a significant risk to achieving this target.
- Target 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all. The article’s finding that “more than two-thirds of rural hospitals in eight states were without obstetric services” demonstrates a clear reduction in “access to quality essential health-care services” for a significant portion of the population.
SDG 10: Reduced Inequalities
- Target 10.2: By 2030, empower and promote the social, economic and political inclusion of all, irrespective of age, sex, disability, race, ethnicity, origin, religion or economic or other status. The article highlights a growing inequality based on geographic location (“other status”). The finding that “12 states experiencing 25% or more losses of obstetric services in rural hospitals” compared to fewer urban losses shows a clear disparity in service provision, undermining the principle of equal access for all.
SDG 5: Gender Equality
- Target 5.6: Ensure universal access to sexual and reproductive health and reproductive rights. Obstetric care is a fundamental part of sexual and reproductive health services. The nationwide decline in these services, as documented in the article, represents a direct barrier to achieving universal access for women.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
Yes, the article provides specific quantitative data that can serve as direct indicators to measure the availability of essential health services.
- Indicator for Targets 3.1, 3.8, and 5.6: The availability of essential health services. The article measures this through:
- The percentage of hospitals that have ceased providing obstetric services. The article states, “seven states had at least 25% of their hospitals report they are no longer providing obstetric services.” This is a direct measure of declining service availability.
- The percentage of rural hospitals without obstetric services. The article provides the specific data point that “by 2022, more than two-thirds of rural hospitals in eight states were without obstetric services.” This indicator measures the extent of “maternity care deserts” in specific regions.
- Indicator for Target 10.2: The disparity in service availability between different population groups. The article implies this indicator by comparing rural and urban data:
- Comparison of service loss in urban vs. rural hospitals. The article notes that while “25% or more of their urban hospitals no longer reported providing obstetric services” in five states, this trend was “more pronounced in rural areas, with a total of 12 states experiencing 25% or more losses of obstetric services in rural hospitals.” The difference between these figures serves as an indicator of geographic inequality in healthcare access.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being |
3.1: Reduce maternal mortality.
3.8: Achieve universal health coverage and access to essential health-care services. |
– Percentage of hospitals (total) that have ceased providing obstetric services. – Percentage of rural hospitals without obstetric services. |
| SDG 10: Reduced Inequalities | 10.2: Promote inclusion and equal access for all, irrespective of status (including geographic location). | – The comparative rate of obstetric service loss between rural and urban hospitals. |
| SDG 5: Gender Equality | 5.6: Ensure universal access to sexual and reproductive health. | – Percentage of hospitals no longer providing obstetric services, as a measure of access to essential reproductive health care for women. |
Source: aha.org
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0