Cardio-Oncology Considerations for Breast Cancer: Risk Stratification, Monitoring, and Treatment – CancerNetwork
Introduction
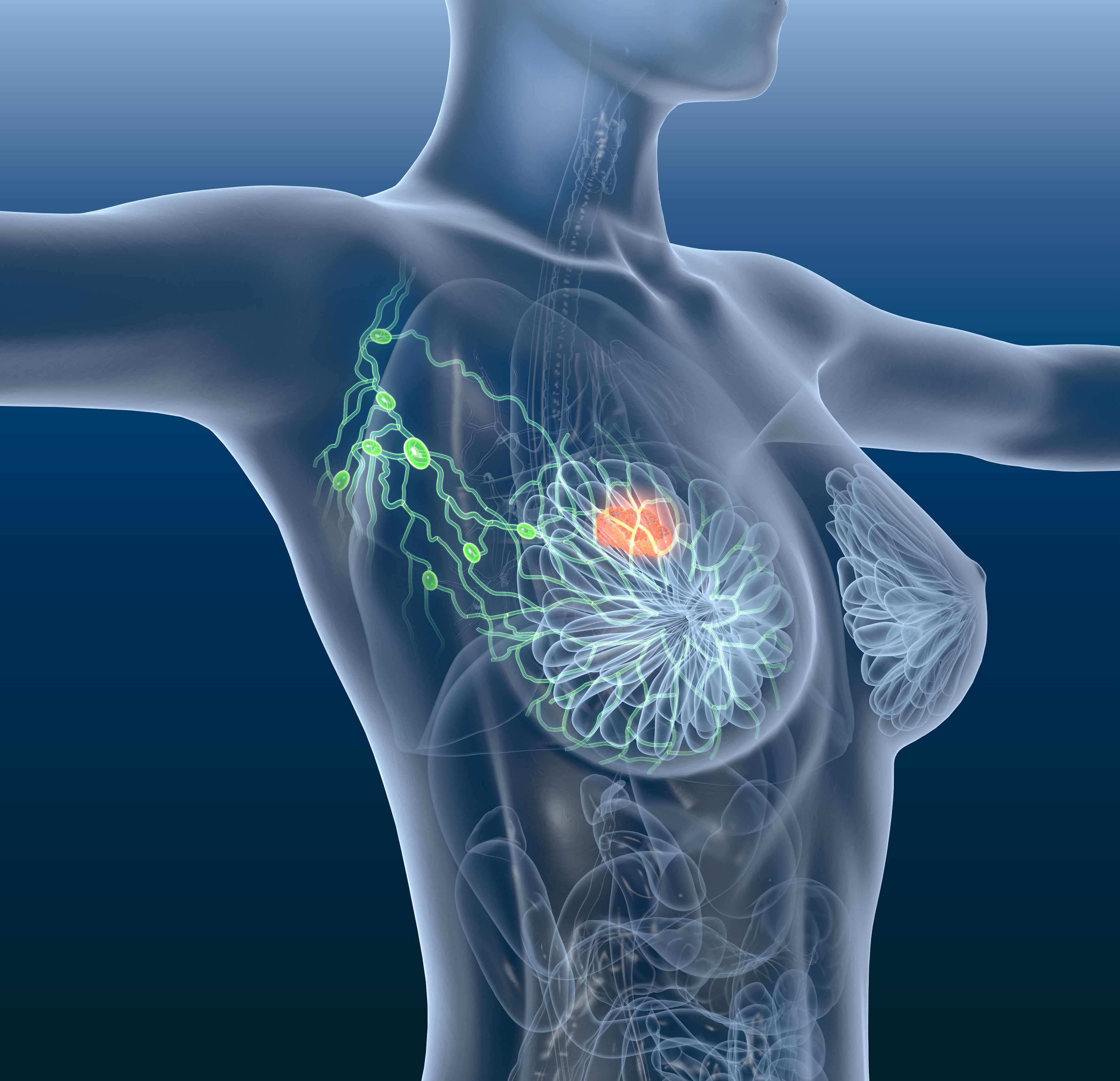
Advancements in breast cancer detection and treatment have significantly improved long-term patient outcomes, with over 4 million women in the US having a prior diagnosis and many now cancer-free. As survival rates increase, non-cancer-related conditions, particularly cardiovascular disease (CVD), have emerged as leading causes of mortality among breast cancer survivors. Studies reveal that breast cancer survivors face nearly double the risk of CVD death compared to age-matched controls, especially those treated with chemotherapy.
Shared risk factors between breast cancer and CVD include age, increased body mass index, decreased physical activity, and alcohol use. Additionally, breast cancer treatments, such as chemotherapy and targeted therapies, contribute to increased cardiovascular risks. This report emphasizes the importance of Sustainable Development Goals (SDGs), particularly SDG 3 (Good Health and Well-being), in addressing these challenges through improved healthcare strategies and patient management.
Treatment-Specific Cardiotoxicities
1. Anthracyclines
Anthracycline-based chemotherapy, used for over 40 years, remains effective against various breast cancer types but is associated with cardiomyopathy and heart failure risk. The cardiotoxicity mechanism involves oxidative stress and cardiomyocyte toxicity. Risk factors include cumulative dose, age, preexisting cardiovascular conditions, and concurrent therapies.
2. HER2-Targeted Therapies
HER2-positive breast cancers, constituting approximately 15% of cases, are treated with targeted agents like trastuzumab and pertuzumab. These therapies carry a 3% to 7% risk of cancer therapy-related cardiac dysfunction (CTRCD), which increases when combined with anthracyclines. HER2 cardiomyopathy may be reversible upon treatment cessation. Monitoring guidelines recommend baseline and periodic cardiac assessments.
3. Endocrine Therapies
Hormone receptor–positive breast cancers, representing over 80% of cases, are treated with selective estrogen receptor modulators (SERMs) and aromatase inhibitors (AIs). AIs are linked to increased risks of dyslipidemia, hypertension, and myocardial infarction, while tamoxifen is associated with venous thromboembolism risk. Comparative studies suggest tamoxifen may have a more favorable cardiovascular profile than AIs.
4. Radiation Therapy
Adjuvant radiation improves survival but raises risks of pericardial disease, ischemic heart disease, arrhythmias, and valvular disease. Risks are dose- and location-dependent, with left breast radiation posing higher cardiovascular risks. Advances in radiation techniques aim to minimize cardiac exposure, aligning with SDG 3 by promoting safer treatment modalities.
5. CDK4/6 Inhibitors
Used for hormone receptor–positive/HER2-negative metastatic breast cancer, CDK4/6 inhibitors such as ribociclib may cause QT-segment prolongation, necessitating ECG monitoring during therapy.
6. Other Therapies
- 5-Fluorouracil (5FU) and its prodrug capecitabine have been associated with angina, hypertension, and myocardial infarction.
- Immune checkpoint inhibitors (ICIs) like pembrolizumab improve cancer outcomes but may cause rare severe cardiovascular toxicities including myocarditis.
- PARP inhibitors such as olaparib are linked to hypertension and thromboembolism risks.
Risk Stratification
Effective cardiovascular risk stratification is essential to mitigate treatment-related cardiotoxicity. Tools endorsed by the 2022 European Society of Cardiology (ESC) guidelines include:
- SMART risk score
- ADVANCE risk score
- SCORE2 and SCORE2-OP
- ASCVD risk score
The International Cardio-Oncology Society (ICOS) and Heart Failure Association (HFA) have developed proformas categorizing patients into low, medium, high, or very high cardiovascular risk, facilitating personalized management. Breast cancer–specific nomograms further aid in predicting cardiotoxicity risk, supporting SDG 3 by enhancing patient-centered care.
Emerging nontraditional cardiovascular risk factors, particularly those unique to women (e.g., preeclampsia, autoimmune diseases), require further research to improve risk assessment accuracy.
Monitoring
Baseline Assessment
- Baseline electrocardiogram (ECG) and transthoracic echocardiogram (TTE) are recommended before initiating anthracycline or HER2-targeted therapies.
- High-risk patients should undergo baseline cardiac biomarker measurements (troponin, natriuretic peptides) to detect subclinical dysfunction.
Monitoring During Treatment
- Periodic ECGs for patients on QT-prolonging agents such as ribociclib.
- Routine TTE to assess left ventricular ejection fraction (LVEF) and global longitudinal strain (GLS) for early detection of cardiotoxicity.
- Cardiac magnetic resonance imaging (CMR) as an adjunctive tool when echocardiographic images are suboptimal.
- Cardiac biomarkers may assist in risk stratification, though their predictive value requires further validation.
Monitoring After Treatment
- Late-onset cardiac dysfunction is a concern, especially in patients treated with anthracyclines or HER2-targeted therapies.
- Follow-up TTE and biomarker assessments within 12 months post-treatment are advised.
- Noninvasive coronary artery disease screening every 5-10 years for patients exposed to significant cardiac radiation doses.
- Patient education on lifestyle modifications and symptom recognition supports long-term cardiovascular health.
Prevention and Treatment
Neurohormonal Agents
Studies on β-blockers, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers show mixed results in preventing cardiotoxicity. Some trials indicate modest benefits, while others show no significant impact. Emerging data suggest sacubitril/valsartan may preserve cardiac function in high-risk patients.
Statins
Evidence on statins for cardiotoxicity prevention is conflicting. Some trials report no significant benefit, whereas others suggest reduced incidence of cardiac dysfunction, highlighting the need for further research.
Dexrazoxane
Dexrazoxane is the only FDA-approved agent for preventing anthracycline-induced cardiotoxicity, demonstrating cardioprotective effects without increasing cancer progression risks.
Adjustment of Anthracycline Administration
- Continuous slow infusion and liposomal formulations reduce cardiotoxicity compared to rapid bolus administration.
- These strategies align with SDG 3 by improving treatment safety and patient outcomes.
Exercise
Exercise may improve cardiorespiratory fitness and attenuate functional disability during chemotherapy, though its role in preventing cardiotoxicity requires further investigation.
Future Directions
Further prospective studies are needed to clarify the role of cardiovascular pharmacotherapy in cardiotoxicity prevention and management. Personalized risk stratification incorporating genetic testing, advanced imaging, and validated risk tools will enhance patient care. These efforts support SDG 3 by promoting health innovation and reducing disease burden.
Conclusion
Cardiotoxicity remains a significant adverse effect of breast cancer treatments, with cardiovascular disease being a leading cause of morbidity and mortality among survivors. Comprehensive risk assessment, monitoring, and preventive strategies are essential to mitigate these risks. Continued research and multidisciplinary collaboration are vital to optimize cardiovascular health in breast cancer patients, advancing the goals of sustainable health and well-being.
1. Sustainable Development Goals (SDGs) Addressed or Connected
- SDG 3: Good Health and Well-being
- The article focuses on improving health outcomes for breast cancer patients, addressing cardiotoxicity and cardiovascular disease risks associated with cancer treatments.
- It emphasizes prevention, monitoring, and management of cardiovascular complications in cancer survivors, aligning with the goal of ensuring healthy lives and promoting well-being for all ages.
- SDG 9: Industry, Innovation, and Infrastructure
- The article discusses advancements in cancer therapies, imaging techniques, and risk stratification tools, reflecting innovation in medical technology and healthcare infrastructure.
- SDG 10: Reduced Inequalities
- By highlighting personalized risk assessment and the need for tailored cardioprotective strategies, the article touches on reducing health inequalities among breast cancer patients with different risk profiles.
- SDG 17: Partnerships for the Goals
- The article references collaborations among international organizations (e.g., ESC, ICOS, NIH), indicating partnerships to improve cardio-oncology care and research.
2. Specific Targets Under Those SDGs Identified
- SDG 3: Good Health and Well-being
- Target 3.4: By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
- The article addresses reducing premature mortality from cardiovascular disease among breast cancer survivors.
- Target 3.8: Achieve universal health coverage, including access to quality essential health-care services and access to safe, effective, quality, and affordable essential medicines and vaccines.
- Focus on access to cardioprotective therapies, monitoring tools, and personalized care aligns with this target.
- Target 3.b: Support the research and development of vaccines and medicines for the communicable and non-communicable diseases that primarily affect developing countries.
- The article emphasizes ongoing research and clinical trials for cardioprotective strategies and cancer therapies.
- Target 3.4: By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
- SDG 9: Industry, Innovation, and Infrastructure
- Target 9.5: Enhance scientific research, upgrade the technological capabilities of industrial sectors, including health technologies.
- Development of new imaging techniques, risk assessment tools, and innovative therapies mentioned in the article support this target.
- Target 9.5: Enhance scientific research, upgrade the technological capabilities of industrial sectors, including health technologies.
- SDG 10: Reduced Inequalities
- Target 10.2: Empower and promote the social, economic and political inclusion of all irrespective of age, sex, disability, race, ethnicity, origin, religion or economic or other status.
- Personalized risk stratification and tailored treatment approaches help address disparities in healthcare outcomes.
- Target 10.2: Empower and promote the social, economic and political inclusion of all irrespective of age, sex, disability, race, ethnicity, origin, religion or economic or other status.
- SDG 17: Partnerships for the Goals
- Target 17.6: Enhance North-South, South-South and triangular regional and international cooperation on and access to science, technology and innovation.
- References to international guidelines and collaborative research efforts reflect this target.
- Target 17.6: Enhance North-South, South-South and triangular regional and international cooperation on and access to science, technology and innovation.
3. Indicators Mentioned or Implied to Measure Progress
- Cardiovascular Mortality and Morbidity Indicators
- Incidence and risk of cardiovascular disease (CVD) mortality among breast cancer survivors compared to controls.
- Rates of heart failure, atrial fibrillation, ischemic heart disease, and other cardiac complications post-treatment.
- Cardiotoxicity Measurement Indicators
- Left ventricular ejection fraction (LVEF) decline of ≥10% to below 53% as a measure of cancer therapy–related cardiac dysfunction (CTRCD).
- Global longitudinal strain (GLS) reductions greater than 12% or 15% from baseline to detect subclinical cardiac dysfunction.
- Biomarkers such as cardiac troponins and natriuretic peptides (BNP/NT-proBNP) levels for early detection of cardiac injury.
- QT-segment prolongation on electrocardiogram (ECG) for monitoring cardiac effects of specific therapies (e.g., CDK4/6 inhibitors).
- Risk Stratification and Monitoring Indicators
- Use of validated cardiovascular risk scores (SMART, ADVANCE, SCORE2, ASCVD) to stratify baseline risk.
- Frequency and results of imaging surveillance (TTE, CMR) and ECG monitoring during and after treatment.
- Incidence of adverse cardiac events in clinical trials evaluating cardioprotective interventions.
- Research and Clinical Trial Indicators
- Outcomes from randomized controlled trials on cardioprotective agents (β-blockers, ACE inhibitors, statins, dexrazoxane).
- Effectiveness of new therapies and monitoring strategies in reducing cardiotoxicity and improving survival.
4. Table: SDGs, Targets and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being |
|
|
| SDG 9: Industry, Innovation, and Infrastructure |
|
|
| SDG 10: Reduced Inequalities |
|
|
| SDG 17: Partnerships for the Goals |
|
|
Source: cancernetwork.com








