We are All Immigrants Now: Trump’s Big Beautiful Bill Decimates Health Care Access for All but a Privileged Few – Milbank Memorial Fund

Report on United States Healthcare Legislation and its Implications for Sustainable Development Goals
Introduction
This report analyzes recent healthcare legislation in the United States, specifically the “Big Beautiful Bill” (BBB), and its significant implications for the nation’s progress toward the United Nations Sustainable Development Goals (SDGs). The legislation, which includes substantial cuts to Medicaid and modifications to the Affordable Care Act (ACA), directly challenges the principles of SDG 3 (Good Health and Well-being), SDG 10 (Reduced Inequalities), and other related goals.
Impact on SDG 3: Good Health and Well-being
Erosion of Universal Health Coverage (Target 3.8)
The legislation represents a significant setback for achieving universal health coverage. The policy changes are projected to have severe consequences for public health infrastructure and individual access to care.
- An estimated 17 million Americans are projected to lose health insurance coverage due to expiring ACA subsidies and Medicaid cuts.
- Reductions in Medicaid Provider taxes are expected to cause financial instability for healthcare facilities, likely resulting in hospital closures, particularly in vulnerable communities.
- The healthcare sector faces significant job losses, with an estimated 500,000 positions at risk, undermining the capacity of the health system.
Creation of Barriers to Healthcare Access
Non-budgetary changes within the legislation create additional obstacles for individuals seeking to obtain or maintain health coverage, further distancing the system from the goals of SDG 3.
- The termination of automatic reenrollment processes increases the administrative burden on individuals.
- Coverage delays for significant life events, such as job loss or childbirth, leave individuals uninsured during critical periods.
- Shortened enrollment periods reduce the window of opportunity for citizens to secure health insurance.
Impact on SDG 10: Reduced Inequalities
Disproportionate Effects on Vulnerable Populations (Target 10.2)
The negative impacts of the BBB are not distributed evenly, exacerbating existing inequalities within the country. This directly contravenes the objective of promoting social and economic inclusion.
- Individuals in rural areas and states with less robust social safety nets are expected to be the most severely affected.
- The policy framework continues a historical trend of restricting access to social safety nets, which began with policies targeting immigrant populations and now extends to a broader demographic of low-income citizens.
- The concept of “racialized legal status” is highlighted, wherein the intersection of race, ethnicity, and perceived legal status creates systemic barriers to healthcare access, even for citizens.
Wider Socio-Economic Repercussions on SDGs
Undermining SDG 1 (No Poverty) and SDG 8 (Decent Work and Economic Growth)
The legislation’s consequences extend beyond the health sector, threatening economic stability and social protection systems.
- SDG 1: The loss of health coverage exposes millions to the risk of catastrophic medical expenses, a primary driver of poverty. This weakens social protection systems (Target 1.3).
- SDG 8: The projected loss of approximately 500,000 healthcare jobs directly contradicts the goal of achieving full and productive employment and decent work for all (Target 8.5).
Challenges to SDG 16: Peace, Justice and Strong Institutions
The legislation introduces measures that weaken the effectiveness and accessibility of public institutions responsible for administering health benefits.
- Increased administrative burdens, including complex paperwork and stringent identity verification processes, create systemic obstacles that can lead to eligible individuals losing their coverage.
- Reduced funding for healthcare navigators and Medicaid staff diminishes the institutional support available to help citizens navigate the complex enrollment process, undermining the development of effective and accountable institutions (Target 16.6).
Key Findings on Systemic Barriers to Health Access
Field research highlights three critical outcomes of the policy direction that impede progress on the SDGs:
- Deterrence of Health-Seeking Behavior: Increased funding for immigration enforcement creates a climate of fear that discourages individuals, including citizens in mixed-status families, from seeking essential medical care. This directly undermines public health objectives central to SDG 3.
- Coverage Loss from Administrative Hurdles: New administrative requirements for Medicaid result in coverage loss for eligible individuals due to procedural complexities and errors. This reflects a failure of institutional accessibility, as outlined in SDG 16.
- Increased Vulnerability Due to State Fiscal Pressure: Federal budget cuts transfer fiscal strain to state governments, which may be forced to curtail health programs for the most vulnerable populations. This trend threatens to deepen inequalities, in opposition to the core principles of SDG 10.
Analysis of SDGs, Targets, and Indicators
1. Which SDGs are addressed or connected to the issues highlighted in the article?
The article discusses issues related to healthcare access, inequality, poverty, and employment, which connect to several Sustainable Development Goals (SDGs). The following SDGs are most relevant:
- SDG 3: Good Health and Well-being: The core theme of the article is the erosion of healthcare access and coverage due to policy changes like the “Big Beautiful Bill” (BBB), which directly impacts the health and well-being of millions.
- SDG 10: Reduced Inequalities: The article emphasizes that the negative impacts of these healthcare cuts disproportionately affect vulnerable and marginalized groups, including immigrants (documented and undocumented), low-income individuals, people of color, and those in rural areas. This highlights the widening gap in healthcare access based on socioeconomic status, race, and legal status.
- SDG 1: No Poverty: By cutting access to affordable healthcare through Medicaid and ACA subsidies, the policies discussed increase the risk of financial hardship and poverty. The article notes that individuals losing coverage can accumulate significant medical debt, pushing them into poverty.
- SDG 8: Decent Work and Economic Growth: The article explicitly states that the proposed cuts to Medicaid could lead to significant job losses in the healthcare sector, directly impacting employment and economic stability.
- SDG 16: Peace, Justice and Strong Institutions: The article touches upon institutional failures, such as increased administrative burdens, confusing enrollment processes, and reduced funding for support systems like healthcare navigators. These issues undermine the effectiveness and accessibility of public institutions responsible for delivering social services.
2. What specific targets under those SDGs can be identified based on the article’s content?
Based on the article’s discussion, several specific SDG targets can be identified:
- Target 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
- The article’s central argument is that the BBB and associated cuts move the country away from this target by causing an estimated “17 million Americans” to lose their health coverage and by eroding the progress made by the Affordable Care Act (ACA) in extending access.
- Target 10.2: By 2030, empower and promote the social, economic and political inclusion of all, irrespective of age, sex, disability, race, ethnicity, origin, religion or economic or other status.
- The article details how policies have systematically excluded immigrants from the social safety net since the 1970s and how the new cuts will particularly harm “immigrants, low-income individuals,” and people of color through concepts like “racialized legal status.”
- Target 10.3: Ensure equal opportunity and reduce inequalities of outcome, including by eliminating discriminatory laws, policies and practices.
- The article critiques policies like the Personal Responsibility and Work Opportunity Act (PRWORA) and the BBB as practices that create and worsen inequalities in health outcomes by targeting specific populations for exclusion from benefits.
- Target 1.3: Implement nationally appropriate social protection systems and measures for all, including floors, and by 2030 achieve substantial coverage of the poor and the vulnerable.
- The article describes Medicaid and ACA subsidies as key components of the “social safety net.” The proposed cuts represent a direct dismantling of this social protection system, reducing coverage for the most vulnerable populations.
- Target 8.5: By 2030, achieve full and productive employment and decent work for all women and men.
- The article directly links the healthcare cuts to negative employment outcomes, stating that “About 500,000 health care jobs could also be lost,” which is a direct setback to this target.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
The article provides several quantitative and qualitative indicators that can be used to measure progress (or regression) towards the identified targets:
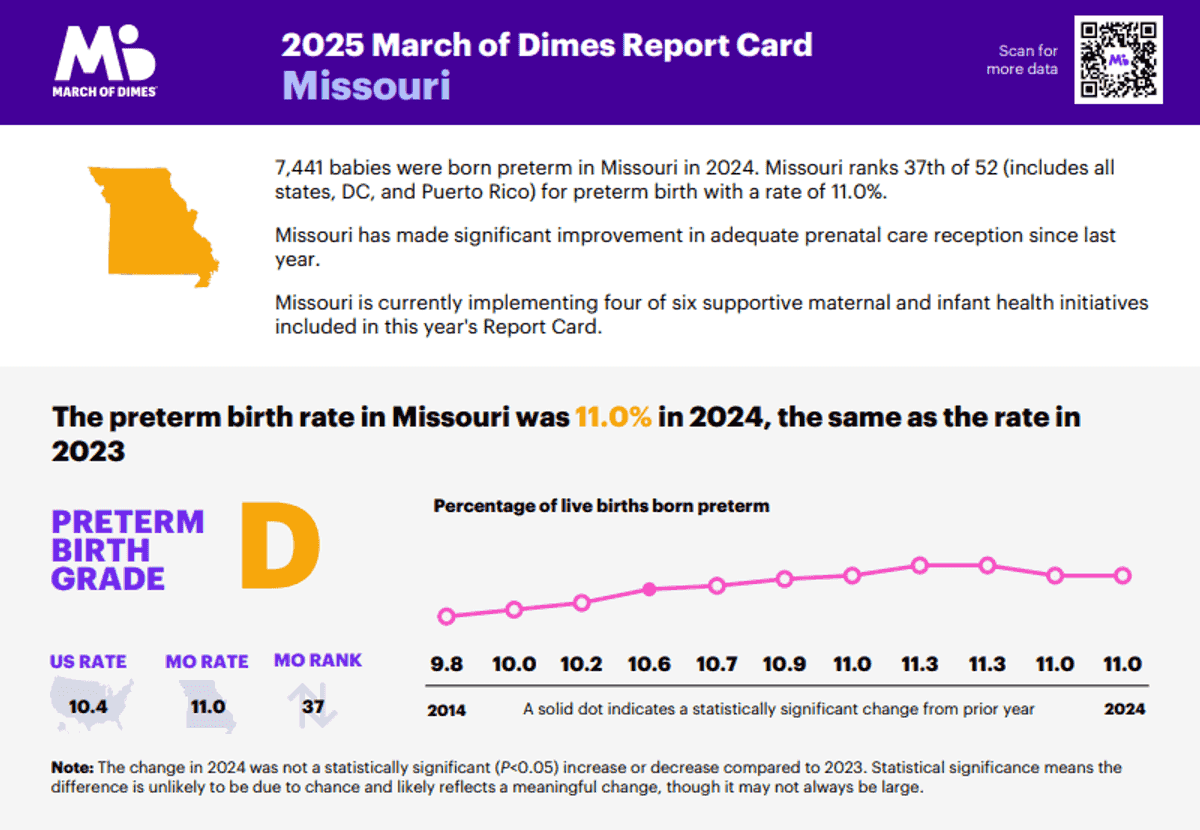
- For Target 3.8 (Universal Health Coverage):
- Number of people with health insurance coverage: The article explicitly states that an estimated “17 million Americans” could lose their coverage, serving as a direct indicator of declining universal health coverage.
- Financial burden of healthcare: The story of Magna, who accumulated “close to $2,000 in bills,” is an indicator of the lack of financial risk protection and an increase in out-of-pocket health expenditures for individuals.
- For Target 10.2 & 10.3 (Reduced Inequalities):
- Proportion of specific populations with access to social benefits: The article implies this indicator by noting that “most immigrants – undocumented and documented – were barred” from ACA provisions. Tracking the percentage of immigrants, low-income families, or racial minorities covered by health insurance would measure this.
- Health-seeking behaviors among vulnerable groups: The article describes how increased immigration enforcement leads to immigrants canceling medical appointments, indicating a reduction in access to care driven by fear and discriminatory practices.
- For Target 8.5 (Decent Work and Economic Growth):
- Number of jobs in the healthcare sector: The projection that “500,000 health care jobs could also be lost” is a direct, quantifiable indicator related to employment.
- For Target 1.3 (Social Protection):
- Coverage of social protection programs: The reduction in the number of people enrolled in Medicaid and receiving ACA subsidies is a primary indicator of the shrinking social safety net.
- For Target 16.6 (Strong Institutions):
- Accessibility and efficiency of public services: The article implies indicators such as application error rates (“erroneous eligibility decision”), the complexity of paperwork (“confusing paperwork”), and the availability of institutional support (reduction in funding for “health care navigators”).
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators Identified in the Article |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.8: Achieve universal health coverage, including financial risk protection and access to quality essential health-care services. |
|
| SDG 10: Reduced Inequalities | 10.2: Promote the social, economic, and political inclusion of all. 10.3: Ensure equal opportunity and reduce inequalities of outcome. |
|
| SDG 1: No Poverty | 1.3: Implement nationally appropriate social protection systems for all, achieving substantial coverage of the poor and vulnerable. |
|
| SDG 8: Decent Work and Economic Growth | 8.5: Achieve full and productive employment and decent work for all. |
|
| SDG 16: Peace, Justice and Strong Institutions | 16.6: Develop effective, accountable and transparent institutions at all levels. |
|
Source: milbank.org

What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0








/campaigns/16-days-of-activism-against-gender-based-violence/pr-web-banner.tmb-1200v.jpg?sfvrsn=8cc7b98e_1#)