PCOS, race, and obesity drive hypertension and metabolic risk – Contemporary OB/GYN

Report on Cardiovascular and Metabolic Health Disparities in Reproductive-Aged Women
Introduction: Aligning Women’s Health Research with Sustainable Development Goals
A recent study examining the interplay between Polycystic Ovary Syndrome (PCOS), race, and obesity reveals significant health disparities that directly impact the achievement of several United Nations Sustainable Development Goals (SDGs). The findings underscore critical challenges to SDG 3 (Good Health and Well-being) by highlighting risk factors for non-communicable diseases, SDG 5 (Gender Equality) by focusing on a health condition specific to women, and SDG 10 (Reduced Inequalities) by exposing stark racial disparities in health outcomes. This report synthesizes the study’s findings, framing them within the context of these global development objectives.
Study Overview and Key Health Indicators
Methodology
The case-control study analyzed the health data of reproductive-aged women to determine the influence of PCOS, race, and obesity on cardiovascular and metabolic risk factors. Key parameters included:
- Blood Pressure (BP) and Body Mass Index (BMI) measurements.
- Classification of participants by PCOS status.
- Demographic categorization, including non-Hispanic Black, non-Hispanic White, and Hispanic.
- Assessment of pre-metabolic syndrome (pre-MetS), defined as the coexistence of obesity and pre-hypertension or hypertension.
Obesity and Hypertension Classifications
The study utilized established clinical classifications to measure health risks, which are critical for monitoring progress toward SDG 3 targets on non-communicable diseases.
- Obesity Classes:
- Class 1: BMI of 30 to
- Class 2: BMI of 35 to
- Class 3: BMI of ≥40 kg/m²
- Hypertension (HTN) Stages:
- Stage 1 HTN
- Stage 2 HTN
Analysis of Findings in Relation to SDG 3: Good Health and Well-being
The Impact of PCOS and Obesity on Non-Communicable Disease Risk
The research demonstrates that PCOS is a significant contributor to health risks that undermine SDG 3, which aims to reduce premature mortality from non-communicable diseases. The condition is strongly associated with obesity and metabolic dysfunction.
- PCOS and Obesity: Women with PCOS showed significantly higher rates of obesity. After adjusting for demographics, the risk for class 3 (severe) obesity was six times greater in women with PCOS compared to controls.
- PCOS and Pre-Metabolic Syndrome: The odds of meeting the criteria for pre-MetS were 1.65 times higher in patients with PCOS, a risk that doubled after adjusting for age and race.
- Compounded Risk: The combination of PCOS and obesity significantly amplified the risk for hypertension. In obese women with PCOS, the adjusted odds ratio for overall hypertension was 1.36.
Racial Disparities: A Barrier to SDG 10 (Reduced Inequalities)
Independent Influence of Race on Health Outcomes
A primary finding of the study is the persistent racial inequality in health outcomes, a direct challenge to the objective of SDG 10 to reduce inequality within and among countries. These disparities were observed independently of PCOS status, indicating systemic issues in health equity.
- Elevated Risk in Non-Hispanic Black Women: Non-Hispanic Black women demonstrated significantly higher odds of hypertension and pre-metabolic syndrome, regardless of whether they had PCOS.
- Risk in Nonobese Population: Even among nonobese individuals, non-Hispanic Black women had an adjusted odds ratio of 1.57 for overall hypertension, highlighting a risk factor independent of both obesity and PCOS.
- Pre-MetS Disparity: A significant link was found between non-Hispanic Black race and meeting pre-MetS criteria, with an adjusted odds ratio of 1.83.
Conclusion: An Integrated Approach to Health, Gender, and Racial Equity
The study’s findings confirm that PCOS, obesity, and race are critical, intersecting determinants of cardiovascular and metabolic health in women. Addressing these challenges is essential for making substantive progress on the Sustainable Development Goals. The following conclusions are drawn:
- Advancing SDG 3 and SDG 5: Targeted health interventions for women with PCOS are necessary to mitigate their predisposition to obesity and hypertension, thereby contributing to better health outcomes (SDG 3) and addressing a key issue in women’s health (SDG 5).
- Fulfilling the Mandate of SDG 10: The pronounced health risks faced by non-Hispanic Black women, independent of other factors, demand public health strategies that actively work to dismantle systemic racial inequalities in healthcare.
- Integrated Policy Action: Progress toward global health and equality goals requires an integrated approach that recognizes and addresses the compounded impact of gender-specific conditions, metabolic health, and racial background.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
- SDG 3: Good Health and Well-being: The article’s primary focus is on health conditions such as Polycystic Ovary Syndrome (PCOS), hypertension (HTN), obesity, and pre-metabolic syndrome (MetS), which are significant risk factors for cardiovascular disease (CVD). It directly addresses the health and well-being of reproductive-aged women.
- SDG 5: Gender Equality: The research specifically centers on women’s health issues, examining conditions like PCOS that exclusively affect women. By highlighting health disparities and risks within the female population, it contributes to the broader goal of ensuring women’s health and well-being, which is a component of gender equality.
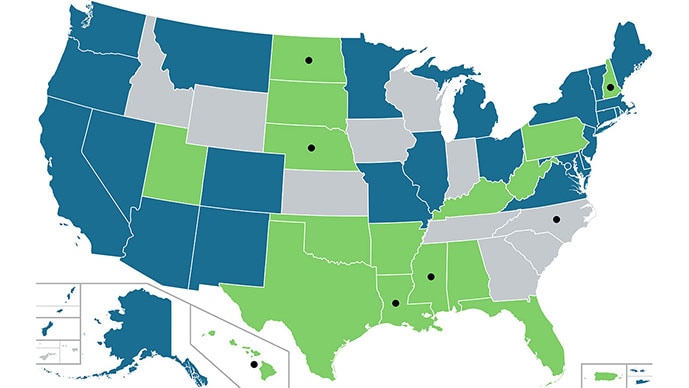
- SDG 10: Reduced Inequalities: A central theme of the article is the racial disparity in health outcomes. It repeatedly emphasizes that non-Hispanic Black (NHB) women face significantly higher health risks for hypertension and pre-metabolic syndrome, independent of other factors like PCOS. This directly addresses the goal of reducing inequalities based on race and ethnicity.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Under SDG 3 (Good Health and Well-being):
- Target 3.4: By 2030, reduce by one-third premature mortality from non-communicable diseases (NCDs) through prevention and treatment and promote mental health and well-being. The article investigates key NCDs and risk factors, including hypertension, obesity, and cardiovascular disease, which is noted as “the leading cause of death among US women.” The study’s focus on identifying high-risk populations is crucial for prevention strategies.
-
Under SDG 10 (Reduced Inequalities):
- Target 10.2: By 2030, empower and promote the social, economic and political inclusion of all, irrespective of age, sex, disability, race, ethnicity, origin, religion or economic or other status. The article highlights health inequalities based on race, showing that “Non-Hispanic Black women had significantly higher odds of hypertension and pre-metabolic syndrome.” This points to a lack of equitable health outcomes for a specific racial group.
- Target 10.3: Ensure equal opportunity and reduce inequalities of outcome, including by eliminating discriminatory policies and practices. The research provides evidence of “inequalities of outcome” in health, demonstrating that “Racial disparities persisted independent of PCOS.” Such data is essential for developing policies to address and reduce these health outcome gaps.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
For Target 3.4 (Reduce mortality from NCDs):
- Prevalence of hypertension: The article measures and reports on different stages of hypertension, such as “Stage 1 HTN” and “overall HTN.” The odds ratios (OR) for hypertension (e.g., “Adjusted ORs for overall HTN…were 1.36”) serve as specific metrics.
- Prevalence of obesity: The study uses Body Mass Index (BMI) to classify patients into different obesity classes (“Class 1,” “Class 2,” and “Class 3 obesity”). The finding of a “6-fold increased risk of class 3 obesity” in PCOS cases is a quantifiable indicator.
- Prevalence of pre-metabolic syndrome (pre-MetS): The article explicitly measures the rate of pre-MetS, noting that it was “more common in women with PCOS, with risk doubling when accounting for age and race.”
-
For Targets 10.2 and 10.3 (Reduce inequalities):
- Health outcome data disaggregated by race: The core of the article’s analysis relies on comparing health data across racial groups (“NHB, non-Hispanic White, and Hispanic”). This disaggregation is a key method for monitoring inequalities.
- Odds Ratios (OR) comparing racial groups: The article uses adjusted odds ratios as direct indicators of disparity. For example, the “adjusted OR for overall HTN of 1.57…for NHB race” and the “adjusted OR of 1.83” for pre-MetS in NHB women quantify the extent of the health inequality compared to other racial groups.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | Target 3.4: Reduce premature mortality from non-communicable diseases (NCDs). |
|
| SDG 10: Reduced Inequalities | Target 10.2: Promote inclusion of all, irrespective of race, ethnicity, etc.
Target 10.3: Ensure equal opportunity and reduce inequalities of outcome. |
|
Source: contemporaryobgyn.net
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0