Hemoglobin glycation index and neutrophil percentage as predictors of congestive heart failure among individuals diagnosed with sepsis: A MIMIC-IV cohort study – Nature
Abstract: Advancing SDG 3 Through Predictive Health Analytics
In alignment with Sustainable Development Goal 3 (Good Health and Well-being), particularly Target 3.4 aimed at reducing premature mortality from non-communicable diseases, this study investigates a novel combined biomarker for predicting Congestive Heart Failure (CHF) in sepsis patients. The research analyzed data from 11,089 adult sepsis patients from the MIMIC-IV database. A combined indicator, integrating the Hemoglobin Glycation Index (HGI) and neutrophil percentage, was developed and evaluated. Results demonstrate that this indicator is a significant and independent risk factor for developing CHF. Patients with higher levels of the combined indicator showed a markedly elevated risk of both CHF (P
1.0 Introduction: The Imperative for Improved Diagnostics in Sepsis Management
1.1 Contextualizing Sepsis and CHF within SDG 3
Sepsis represents a formidable global health challenge, contributing significantly to in-hospital mortality and impeding progress towards Sustainable Development Goal 3 (Good Health and Well-being). The development of complications such as Congestive Heart Failure (CHF) during sepsis drastically worsens patient prognosis and increases the burden on healthcare systems. Achieving SDG Target 3.4, which seeks to reduce premature mortality, necessitates the development of superior tools for the early identification and management of high-risk patients. This study addresses this need by exploring biomarkers that reflect the complex interplay of metabolic dysregulation and inflammation in sepsis.
1.2 A Novel Biomarker for Enhanced Risk Stratification
Current predictors of cardiovascular events often lack comprehensive insight into a patient’s long-term glycemic control and acute inflammatory state. This research proposes and evaluates a combined indicator that integrates two key biomarkers:
- Hemoglobin Glycation Index (HGI): An emerging marker that reflects chronic glycemic variability and is linked to inflammatory processes.
- Neutrophil Percentage: A well-established indicator of acute inflammation and immune response, critical in the pathophysiology of sepsis.
By combining these metrics, this study hypothesizes that a more robust and clinically relevant predictor for CHF in sepsis patients can be established, thereby enhancing the quality of essential healthcare services as outlined in SDG Target 3.8.
2.0 Methodology: A Retrospective Cohort Analysis
2.1 Data Source and Patient Cohort
This retrospective study utilized data from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database. A cohort of 11,089 patients was established based on the following criteria:
- Adult patients (≥ 18 years) meeting Sepsis-3 diagnostic criteria.
- First-time admission to the Intensive Care Unit (ICU).
- ICU stay exceeding 24 hours.
- Availability of key laboratory data (HbA1c, FBG, and neutrophils).
The use of this large, high-quality database ensures the robustness of findings, which is essential for developing evidence-based practices that support the SDGs.
2.2 Definition of the Combined Indicator and Outcomes
The Hemoglobin Glycation Index (HGI) was calculated as the difference between measured HbA1c and predicted HbA1c (Predicted HbA1c = 5.24 + 0.0095 × FBG). Patients were stratified into four quartiles (Q1-Q4) based on a combination of their HGI and neutrophil percentage levels (low/low, low/high, high/low, high/high). The primary outcomes measured were the risk of developing CHF during hospitalization and in-hospital mortality.
2.3 Statistical Analysis
A comprehensive statistical analysis was performed to assess the relationship between the combined indicator and patient outcomes. The methods included:
- Kaplan-Meier (KM) survival curve analysis.
- Multivariable Cox proportional hazards regression models to adjust for confounding variables.
- Restricted Cubic Spline (RCS) analysis to explore non-linear relationships.
3.0 Results: The Predictive Power of the Combined Indicator
3.1 Baseline Characteristics and Cumulative Incidence
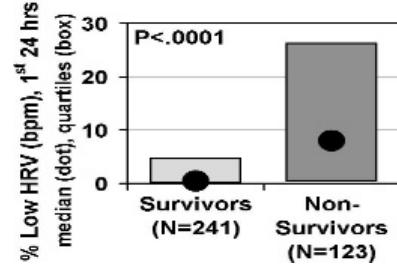
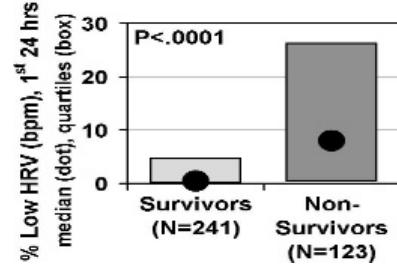
The study cohort of 11,089 patients had a CHF incidence of 30.43%. Significant differences were observed across the four quartiles of the combined indicator in variables such as age, comorbidities (diabetes, myocardial infarction), and severity scores. Cumulative incidence analysis revealed that patients in the highest quartile (Q4) had a significantly higher risk of developing CHF compared to those in the lowest quartile (Q1) (P
3.2 Multivariable Cox Regression Analysis
After adjusting for a comprehensive set of confounding factors (including demographics, comorbidities, and severity scores), the combined indicator remained a strong and independent predictor of CHF. Key findings from the fully adjusted model include:
- Patients in higher quartiles (Q2, Q3, Q4) demonstrated a progressively increased risk of CHF compared to the reference group (Q1).
- Factors associated with a higher CHF risk included a history of myocardial infarction and chronic pulmonary disease.
- Factors associated with a lower CHF risk included being aged ≤ 65 years and being married.
These results underscore the indicator’s utility in identifying vulnerable populations, a critical step for targeted interventions aligned with SDG 3.
3.3 Non-Linear Relationship Analysis (RCS)
RCS analysis revealed a significant non-linear relationship between HGI and CHF risk. The risk increased steadily with rising HGI values, reinforcing that poor long-term glycemic control is a critical factor in cardiac complications during sepsis. This nuanced understanding supports the development of more precise clinical guidelines.
4.0 Discussion: Implications for Global Health and SDG 3
The findings of this study have significant implications for clinical practice and the pursuit of SDG 3. The combined indicator, integrating both chronic metabolic health (HGI) and acute inflammatory status (neutrophil percentage), offers a more holistic and powerful tool for risk stratification than either marker alone. This integrated approach directly supports SDG Target 3.4 by enabling the early identification of sepsis patients at high risk of CHF, allowing for preemptive monitoring and intervention to reduce premature mortality.
By providing a low-cost, data-driven tool derived from commonly available laboratory tests, this research also contributes to SDG Target 3.8 (Universal Health Coverage) and Target 3.d (Strengthening Early Warning Systems). The ability to better predict severe complications allows for more efficient allocation of healthcare resources, which is crucial in both developed and developing nations. The synergistic effect of high HGI and elevated neutrophil activity highlights a glyco-inflammatory pathway that can be a target for future therapeutic strategies, further advancing the goal of improving health outcomes for all.
5.0 Conclusion and Recommendations
This study successfully demonstrates that a combined indicator of HGI and neutrophil percentage is an independent and significant predictor of congestive heart failure and in-hospital mortality in critically ill sepsis patients. This novel biomarker provides a more accurate risk assessment by capturing both chronic metabolic dysregulation and acute inflammation.
To advance the objectives of Sustainable Development Goal 3, the following recommendations are made:
- Clinical Integration: Healthcare providers should consider monitoring HGI and neutrophil percentage in sepsis patients to identify high-risk individuals for CHF development.
- Targeted Interventions: For patients with elevated levels of the combined indicator, more aggressive management of glycemic control and inflammatory responses may be warranted to mitigate cardiac risk.
- Future Research: Prospective, multicenter studies are needed to validate these findings across diverse populations and to evaluate the effectiveness of interventions based on this risk stratification tool.
Adopting such predictive tools in clinical practice represents a tangible step toward strengthening health systems, reducing premature mortality, and ensuring good health and well-being for all.
1. Which SDGs are addressed or connected to the issues highlighted in the article?
SDG 3: Good Health and Well-being
- The article directly addresses health issues by investigating risk factors for congestive heart failure (CHF) in patients with sepsis. Sepsis is described as a “major global concern in critical care medicine and remains a major contributor to in-hospital mortality.” This aligns with the overall goal of ensuring healthy lives and promoting well-being for all at all ages.
- The research focuses on improving patient outcomes by identifying predictors for severe complications. The study aims to understand the link between a combined biomarker (hemoglobin glycation index and neutrophil percentage) and the “risk of in-hospital mortality” and the “risk of congestive heart failure (CHF),” which are critical health outcomes.
2. What specific targets under those SDGs can be identified based on the article’s content?
Target 3.4: By 2030, reduce by one-third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
- The article focuses on Congestive Heart Failure (CHF), a major non-communicable cardiovascular disease. The study investigates predictors for CHF to enable better “risk stratification” and “early identification of patients at risk.” This contributes directly to the prevention and treatment aspect of the target.
- The study explicitly analyzes “in-hospital mortality risk” and finds that “elevated levels of the combined indicator or HGI were linked to an elevated in-hospital mortality risk.” By identifying these risk factors, the research provides a basis for clinical interventions aimed at reducing mortality from CHF in sepsis patients.
Target 3.d: Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks.
- Sepsis is identified as a “major global concern.” The research aims to develop a more effective method for predicting a severe complication (CHF), which enhances the capacity for risk reduction and management in a critical care setting.
- The conclusion suggests that the “combined indicator may improve identification of high-risk individuals who would benefit from intensive monitoring and early intervention.” This development of a novel predictive tool directly supports the strengthening of capacities for early warning and risk management of a global health threat like sepsis.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
Indicator 3.4.1: Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease.
- The article provides data directly related to this indicator by studying mortality and morbidity from a cardiovascular disease (CHF). It states that the “CHF incidence of 30.43% in the sepsis cohort” was observed.
- It also measures the “in-hospital mortality risk” associated with the condition. The Kaplan-Meier survival curves demonstrated that patients in the highest quartile of the combined indicator “had a lower survival rate,” directly linking the studied biomarkers to mortality outcomes.
Indicator related to Target 3.d (Implied): Capacity for risk reduction and management of health emergencies.
- While the article does not measure national capacity (as in indicator 3.d.1), it contributes a tool to enhance it. The primary outcome is the validation of the “combined indicator (comprising HGI and neutrophil percentage)” as an “independent risk factor for CHF.”
- This indicator can be used in clinical practice for “early detection” and to “identify those at higher risk of CHF,” thereby improving the management of sepsis-related complications. The effectiveness of this predictive tool serves as an implied measure of enhanced capacity for risk reduction.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.4: Reduce by one-third premature mortality from non-communicable diseases through prevention and treatment. | 3.4.1: Mortality rate attributed to cardiovascular disease. The article measures “in-hospital mortality risk” and reports a “CHF incidence of 30.43%” in the study cohort. |
| SDG 3: Good Health and Well-being | 3.d: Strengthen the capacity of all countries… for early warning, risk reduction and management of national and global health risks. | Implied Indicator: Development and use of predictive tools for risk stratification. The article validates a “combined indicator (integrating HGI and neutrophil percentage)” to predict CHF risk in sepsis patients, enhancing clinical management capacity. |
Source: nature.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0