New missions for GLP-1 drugs: Treating alcoholism and smoking? – The Mercury News

Advancing Sustainable Development Goal 3: Novel Pharmaceutical Applications for Substance Use Disorders
Recent research indicates that Glucagon-like peptide-1 (GLP-1) receptor agonists, initially developed for diabetes management and weight loss, show significant potential in treating alcohol and other substance use disorders. This development represents a critical advancement toward achieving the United Nations Sustainable Development Goals, particularly SDG 3, which aims to ensure healthy lives and promote well-being for all at all ages.
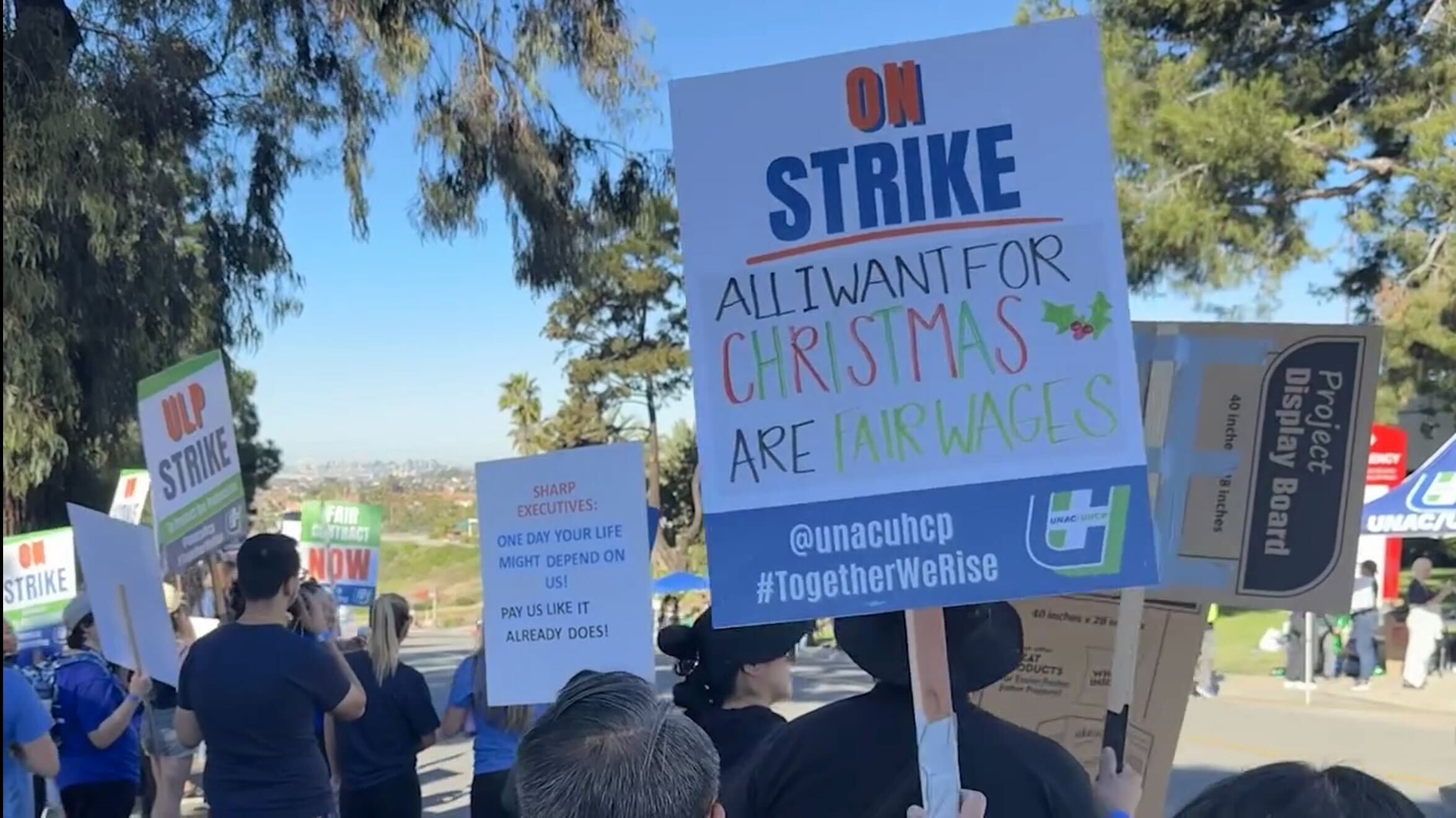
Addressing Target 3.5: Strengthening Prevention and Treatment of Substance Abuse
The harmful use of alcohol presents a major public health challenge, directly impeding progress on SDG Target 3.5. In the United States, the scale of this issue is substantial:
- Alcohol-related diseases result in approximately 178,000 deaths annually.
- This figure is more than double the mortality rate from opioid overdoses, which accounted for around 80,000 deaths in 2024.
The emergence of more effective medical interventions is therefore essential for reducing premature mortality from non-communicable diseases and promoting mental health, in line with SDG Target 3.4.
Clinical and Observational Evidence Supporting GLP-1 Agonists
A growing body of evidence, presented by addiction medicine specialists from UCLA at the California Society of Addiction Medicine conference, highlights the efficacy of GLP-1 drugs in reducing alcohol and substance consumption. These findings offer a promising pathway to enhance treatment for substance use disorders.
Key Research Findings
- A study of 153 obese adults using GLP-1 drugs found significant self-reported reductions in alcohol intake, frequency of binge drinking, and scores on alcohol use disorder assessments.
- A 17-year observational study in Sweden demonstrated that GLP-1 drugs substantially decreased the risk of hospitalizations related to alcohol use disorder among individuals with obesity and Type 2 diabetes.
- A clinical trial involving 48 adults with alcohol use disorder showed that weekly low-dose semaglutide administration significantly reduced alcohol consumption and cravings. A notable secondary finding was a reduction in daily cigarette consumption among participants who smoked.
- An analysis of over 1,500 social media posts related to GLP-1 drugs and alcohol revealed that 71% of users reported reduced alcohol cravings and a decreased desire to drink.
- Pre-clinical rodent studies have corroborated these findings, showing that semaglutide reduced alcohol intake and relapse. Furthermore, another GLP-1 drug, liraglutide, was found to reduce fentanyl-seeking behavior in rats with an efficacy comparable to buprenorphine, the current standard for opioid addiction treatment.
Potential Mechanisms of Action
The precise mechanisms are not fully understood but are believed to involve the modulation of reward pathways in the central nervous system. Additionally, the drugs’ known effect of slowing gastric emptying may contribute by reducing overall alcohol consumption and blunting the rise in blood alcohol content.
Bridging the Treatment Gap to Achieve Universal Health Coverage (SDG Target 3.8)
Despite the promise of new pharmaceuticals, significant barriers exist to implementing effective, science-based addiction treatment, hindering progress toward universal health coverage as outlined in SDG Target 3.8.
Disparities in Pharmaceutical Innovation and Access
- Over the past decade, ten new drugs have been approved by the FDA for diabetes, while only three have been approved for alcohol use disorder in the last 74 years.
- A significant gap persists between scientific evidence and clinical practice. Data from the Substance Abuse and Mental Health Services Administration indicates that just over half of treatment facilities in California offer any form of medication-assisted treatment.
This disparity highlights a systemic challenge in integrating addiction treatment with mainstream medicine. Overcoming the persistent anti-medication bias in some treatment circles is crucial for ensuring that scientific breakthroughs translate into saved lives, aligning with the core mission of SDG 3.
Analysis of the Article in Relation to Sustainable Development Goals
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
The article is fundamentally centered on public health issues. It discusses mortality rates from substance abuse (alcohol and opioids), the prevalence of non-communicable diseases like diabetes and obesity, and the development of new medical treatments to address these health crises. The core theme is the potential of a new class of drugs (GLP-1) to improve health outcomes and save lives by treating addiction, which directly aligns with the goal of ensuring healthy lives and promoting well-being for all.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Target 3.4: By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
The article connects to this target by discussing diseases that cause premature mortality. It explicitly mentions that “alcohol-related diseases kill more than… 178,000 every year” and that the drugs in question were originally designed to “control diabetes.” Both are non-communicable diseases. The research into using these drugs for alcoholism represents a significant potential advancement in treatment, aiming to reduce mortality from this cause.
-
Target 3.5: Strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.
This target is the central focus of the article. The text details the promise of GLP-1 drugs in “treating alcoholism, and perhaps smoking and other substance use disorders as well.” It cites multiple studies showing the drugs lead to “significant reductions in self-reported alcohol intake,” “drops in binge drinking,” and reduced fentanyl-seeking behavior in animal studies. The article also highlights a major gap in current treatment, stating that “only slightly more than half of treatment facilities in California offer any kind of medication-assisted treatment,” underscoring the need to strengthen treatment as outlined in this target.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
- Mortality Rate from Substance Abuse: The article provides direct statistics that can serve as indicators of mortality. It states that “alcohol-related diseases kill… about 178,000 every year” and “some 80,000 Americans died from drug overdoses in 2024.” These figures are direct measures of mortality that new treatments aim to reduce, aligning with Target 3.4.
- Harmful Use of Alcohol: Progress towards reducing the harmful use of alcohol (related to Target 3.5) is implied through the results of the studies mentioned. The article cites findings such as “significant reductions in self-reported alcohol intake,” “fewer drinks per day,” “drops in binge drinking,” and “lower scores on alcohol use disorder tests.” These are all measurable outcomes that can be used as indicators.
- Coverage of Treatment for Substance Use Disorders: The article provides a specific indicator for treatment coverage (related to Target 3.5.1). It states, “only slightly more than half of treatment facilities in California offer any kind of medication-assisted treatment.” This percentage is a direct measure of the availability and coverage of effective scientific treatments for addiction.
- Reduction in Tobacco Use: An indicator for reduced tobacco use is mentioned in the context of a clinical trial where a subgroup of smokers “showed a significant reduction in the consumption of cigarettes per day.” This directly relates to the substance abuse target (3.5).
4. SDGs, Targets and Indicators Table
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.4: Reduce premature mortality from non-communicable diseases through prevention and treatment. |
|
| SDG 3: Good Health and Well-being | 3.5: Strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol. |
|
Source: mercurynews.com

What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0















































:focal(1500,1000)/https://media.globalcitizen.org/a6/9a/a69a4720-d8a1-4715-b596-18738d03c05c/rotary_polio_hero_image.jpg?#)





/countries/sri-lanka/photo-credit---dmc-sri-lanka.tmb-1200v.jpg?sfvrsn=dc298bcc_1#)