Sir Anthony Hopkins quit drinking 50 years ago – what you can learn from his abstinence – Times of India
Report on Alcohol Dependence, Recovery, and Alignment with Sustainable Development Goals
Introduction: Public Health and Sustainable Development
The harmful use of alcohol presents a significant obstacle to achieving the United Nations Sustainable Development Goals (SDGs), particularly SDG 3: Good Health and Well-being. This report examines the mechanisms of alcohol dependence, pathways to recovery, and societal trends through the case study of Sir Anthony Hopkins. His experience provides a framework for understanding the individual and public health dimensions of substance abuse, directly relating to SDG Target 3.5, which aims to strengthen the prevention and treatment of substance abuse, including the harmful use of alcohol.
Case Study: Sir Anthony Hopkins and Spontaneous Remission
Background and Onset of Dependence
Sir Anthony Hopkins’ early life and career were marked by alcohol dependence, a condition he described as a coping mechanism for personal insecurity. This pattern reflects a common pathway to substance use disorders, where alcohol is initially used to mitigate psychological distress. Neuroscience research confirms that chronic alcohol use hijacks the brain’s prefrontal cortex, impairing judgment and embedding a cycle of craving. This neurobiological impact undermines an individual’s capacity for well-being, a core tenet of SDG 3.
The Recovery Turning Point
On December 29, 1975, Hopkins experienced a moment of profound self-awareness that led to immediate and sustained abstinence. This event, described by neuroscientists as spontaneous remission or a “cognitive reframe,” represents a sudden rewiring of neural pathways where denial is overcome. This psychological shift aligns with the promotion of mental health and well-being (SDG Target 3.4), as it marks the beginning of brain healing and the reconstruction of a healthy identity. Research indicates that such transformative moments, often linked to a sense of surrender or spiritual awakening, are correlated with stronger long-term recovery outcomes and a renewed sense of purpose.
Public Health Impact of Alcohol and SDG 3 Targets
Scientific Consensus on Alcohol-Related Harm
Global health authorities have established that no level of alcohol consumption is safe for health, a finding that reinforces the urgency of addressing alcohol as a public health priority under SDG 3. Key findings include:
- The World Health Organization (WHO) and a landmark 2018 study in The Lancet concluded that the safest level of drinking is none.
- The Global Burden of Disease 2020 study identified alcohol as the leading risk factor for premature mortality among individuals aged 15-49.
- The WHO’s Global Strategy for 2024 actively works to dismantle the myth of “moderate safe drinking” that undermines public health initiatives.
Physiological and Psychological Consequences
The detrimental effects of alcohol directly impede progress toward ensuring healthy lives. The physical and mental health consequences create a significant burden on individuals and healthcare systems, contrary to the goals of SDG 3.
- Cardiovascular and Liver Health: Research in the European Heart Journal links even moderate daily alcohol consumption to a 16% increased risk of atrial fibrillation. Long-term use leads to liver damage via toxic acetaldehyde buildup.
- Mental Health: A meta-study in the British Medical Journal found that individuals with alcohol use disorder are five times more likely to develop depression. This comorbidity highlights the need for integrated health services as advocated by SDG 3.
A Framework for Recovery in Line with SDG 3.5
Evidence-Based Strategies for Abstinence and Reduction
Achieving SDG Target 3.5 requires the implementation of accessible, evidence-based recovery strategies. The following steps, supported by public health research, provide a structured approach for individuals seeking to reduce or end their alcohol consumption:
- Medical Consultation: A healthcare professional should supervise withdrawal from heavy or daily alcohol use to manage potentially dangerous symptoms. This step ensures safe detoxification and connects individuals to formal support systems.
- Goal Setting and Progress Monitoring: Clearly defining motivations for quitting and identifying triggers are crucial cognitive-behavioral techniques. Replacing drinking routines with healthy alternatives helps restructure daily life around well-being.
- Integrated Treatment Modalities: A combination of therapy, peer support groups (e.g., AA, SMART Recovery), and, where appropriate, medication (e.g., naltrexone) offers the most effective path to sustained recovery.
- Environmental Restructuring: Modifying one’s environment to remove drinking cues and building new social networks that support sobriety are critical for preventing relapse and fostering a new identity centered on health.
Societal Shifts Toward Health and Well-being
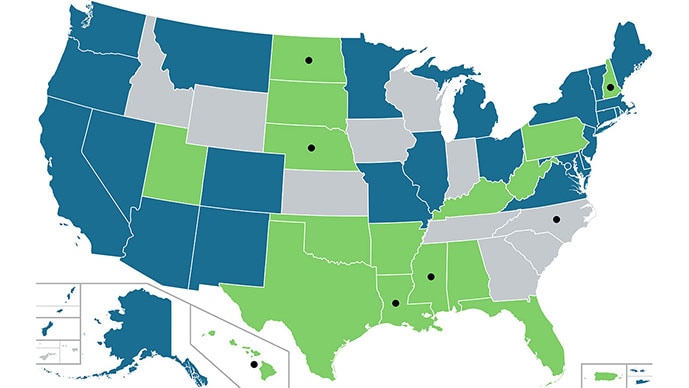
The Rise of the Sober-Curious Movement
A significant cultural shift, particularly among younger generations, is contributing to the goals of SDG 3. The “sober-curious” movement and mindful drinking trends represent a proactive, preventative approach to public health. According to 2023 Gallup data, only 62% of adults under 35 report drinking, a marked decrease from previous decades. This trend is supported by a growing market for non-alcoholic beverages, projected to exceed $30 billion by 2030, and digital health platforms that offer accessible support for recovery. This cultural change normalizes sobriety and aligns with the preventative health focus of the Sustainable Development Goals.
Conclusion: From Individual Recovery to Global Health
Sir Anthony Hopkins’ journey from alcohol dependence to sustained recovery illustrates that healing is possible and transformative. His story, when viewed through the lens of public health, underscores the principles of SDG 3: Good Health and Well-being. The scientific evidence on alcohol’s harm, combined with effective recovery frameworks and positive cultural trends, provides a clear roadmap for action. Addressing the harmful use of alcohol is not merely an individual challenge but a critical component of the global agenda to ensure healthy lives and promote well-being for all.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
- The entire article is centered on health, specifically the negative impacts of alcohol consumption and the journey towards recovery and well-being. It discusses alcohol addiction as a disease, its effects on mental health (depression, suicide risk), and its role in causing non-communicable physical diseases like heart and liver conditions. The narrative also highlights public health warnings from organizations like the WHO and provides guidance on seeking treatment, which are core components of ensuring healthy lives and promoting well-being for all.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Target 3.4: By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
- The article directly connects to this target by detailing how alcohol use contributes to non-communicable diseases. It cites a study from the European Heart Journal linking alcohol to a “16 percent” increased risk of atrial fibrillation and mentions that long-term exposure damages the liver. Furthermore, it addresses the mental health aspect by referencing a British Medical Journal study finding that people with alcohol-use disorder are “five times more likely to develop depression and six times more likely to attempt suicide.” The article also points to the Global Burden of Disease 2020 study, which identifies alcohol as the “leading risk factor for premature death among adults aged 15 to 49.”
-
Target 3.5: Strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.
- This target is central to the article’s theme. The narrative of Sir Anthony Hopkins’s struggle with alcohol dependence exemplifies the “harmful use of alcohol.” The article promotes prevention by citing warnings from the WHO that “No level of alcohol consumption is safe for our health” and highlighting cultural shifts like the “sober-curious” movement. It also explicitly discusses treatment by outlining evidence-based steps to quit drinking, such as seeing a doctor, combining “therapy, support, and medication,” and utilizing peer groups like AA or SMART Recovery.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Yes, the article mentions several quantitative and qualitative indicators.
- Indicator for Premature Mortality (Target 3.4): The article cites the Global Burden of Disease 2020 study, stating that alcohol is the “leading risk factor for premature death among adults aged 15 to 49.” This statistic serves as a direct indicator of alcohol-attributable mortality.
- Indicator for Mental Health (Target 3.4): The statistic from the British Medical Journal that people with alcohol-use disorder are “five times more likely to develop depression and six times more likely to attempt suicide” can be used as an indicator to measure the mental health burden associated with harmful alcohol use.
- Indicator for Alcohol Consumption (Target 3.5): The article provides data from Gallup 2023 showing a decrease in alcohol consumption among younger generations: “only 62% of adults under 35 report drinking, compared to over 70% two decades ago.” This trend serves as an indicator of the effectiveness of prevention strategies and changing social norms.
- Indicator for Treatment and Recovery Outcomes (Target 3.5): The National Institute on Drug Abuse (NIDA) estimate that “roughly 60 percent of recovering drinkers relapse within their first year” is a key indicator for measuring the effectiveness and challenges of substance abuse treatment programs.
SDGs, Targets, and Indicators Summary
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | Target 3.4: Reduce premature mortality from non-communicable diseases and promote mental health and well-being. |
|
| SDG 3: Good Health and Well-being | Target 3.5: Strengthen the prevention and treatment of substance abuse, including harmful use of alcohol. |
|
Source: timesofindia.indiatimes.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0