Diagnostic predictive evaluation of pneumocystis jirovecii pneumonia using digital chest CT analysis combined with clinical features – Frontiers
Report on an AI-Assisted Diagnostic Model for Pneumonia Subtypes
A Contribution to Sustainable Development Goal 3: Good Health and Well-being
This report details the development and validation of a diagnostic prediction model designed to differentiate Pneumocystis jirovecii pneumonia (PJP) from bacterial pneumonia (BP). By integrating Artificial Intelligence (AI)-based digital analysis of chest CT scans with clinical and laboratory data, this research directly supports the achievement of Sustainable Development Goal 3 (SDG 3), which aims to ensure healthy lives and promote well-being for all at all ages. The model enhances diagnostic accuracy, thereby contributing to reduced mortality from communicable diseases (SDG Target 3.3) and strengthening the capacity for early warning and management of global health risks (SDG Target 3.d).
Introduction: The Global Health Challenge of Pneumonia and SDG 3
Pneumonia remains a significant cause of global morbidity and mortality, posing a substantial obstacle to achieving SDG 3. The accurate and timely differentiation between PJP and BP is critical for effective treatment but presents considerable diagnostic challenges. This difficulty can lead to delayed or inappropriate therapy, resulting in higher mortality rates and increased healthcare burdens, undermining progress towards universal health coverage and quality care (SDG Target 3.8). This study addresses this gap by developing an innovative diagnostic tool that aligns with the global imperative to combat communicable diseases and improve health outcomes.
Methodology: A Framework for Enhanced Health Outcomes
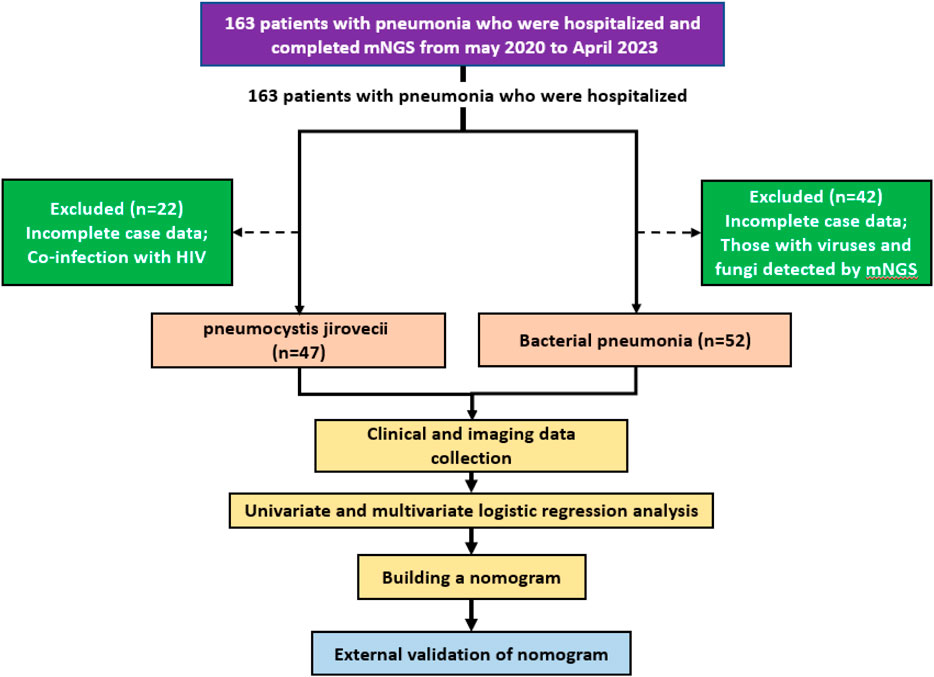
A retrospective, multicenter study was conducted to identify independent predictors of PJP and develop a robust diagnostic model, thereby strengthening evidence-based clinical practice in line with SDG 3 principles.
Study Design and Data Collection
- A training cohort of 99 pneumonia patients and an external validation cohort of 87 patients were established.
- Inclusion and exclusion criteria were strictly applied to create distinct PJP and BP groups, confirmed via metagenomic next-generation sequencing (mNGS).
- Comprehensive data was collected, including:
- Baseline clinical characteristics (demographics, comorbidities, immunosuppressive therapy).
- Laboratory findings within 72 hours of admission (inflammatory markers, biochemistry, blood gas analysis).
- Chest CT imaging data.
- An AI-powered software (Shukun Pneumonia CT Image-Assisted Triage and Evaluation Software) was used for automated, quantitative analysis of CT images, measuring lung and inflammatory lesion volumes and densities.
Statistical Analysis and Model Development
Logistic regression was employed to identify independent predictors of PJP. These predictors were used to construct a nomogram prediction model. The model’s performance was rigorously evaluated for accuracy, calibration, and clinical utility, ensuring its potential to improve the quality of healthcare services as envisioned in SDG 3.
Results: Key Findings for Public Health Advancement
The analysis revealed distinct clinical, laboratory, and imaging profiles for PJP and BP, enabling the development of a highly accurate predictive model that can advance public health goals.
Comparative Analysis of PJP and BP Cohorts
- Clinical Profile: The PJP group had a significantly higher incidence of chronic diseases (93.6% vs. 63.5%) and immunosuppressant use (51.1% vs. 11.5%) compared to the BP group.
- Laboratory Markers: PJP patients exhibited higher LDH levels and lower procalcitonin (PCT), RBC, and CK levels.
- Imaging Findings: AI-assisted CT analysis showed that PJP patients had a significantly greater inflammatory lesion volume (median 952 cm³) compared to BP patients (median 242 cm³), with a predominance in the upper lung lobes.
Development of a Predictive Diagnostic Model
Multivariate logistic regression identified five independent predictors for distinguishing PJP from BP:
- Previous immunomodulator use
- Procalcitonin (PCT) levels
- Ratio of inflammatory lesion volume to total lung volume
- Pneumonia lesion volume in the -700 to -450 HU range
- Pneumonia lesion volume in the -450 to -300 HU range
Model Performance and Validation
The resulting nomogram model demonstrated excellent discriminatory power, a critical step towards strengthening health systems and improving patient outcomes under SDG 3.
- Training Cohort: The model achieved an Area Under the Curve (AUC) of 0.898 and an overall accuracy of 84.2%.
- Validation Cohort: External validation confirmed the model’s robustness, with an AUC of 0.820 and an accuracy of 81.6%.
- Clinical Utility: Decision Curve Analysis (DCA) showed that the model provides a significant net clinical benefit across a range of risk thresholds, supporting its application in clinical decision-making to improve health for all.
Discussion: Implications for Global Health and SDG 3
This study’s primary innovation—the use of a quantitative, AI-driven analysis of CT images combined with clinical data—represents a significant advancement in infectious disease diagnostics. By providing an objective and reliable method to differentiate pneumonia pathogens, this approach directly supports several targets within SDG 3.
- Strengthening Early Warning Systems (SDG Target 3.d): The model serves as a powerful tool for the early and accurate identification of PJP, enabling timely intervention and management of a serious health risk, particularly in vulnerable, immunocompromised populations.
- Combating Communicable Diseases (SDG Target 3.3): By facilitating accurate diagnosis, the model supports targeted antimicrobial therapy. This improves patient outcomes, reduces mortality from pneumonia, and aids in antimicrobial stewardship by avoiding the misuse of antibiotics.
- Enhancing Quality of Care (SDG Target 3.8): The integration of AI technology into clinical workflows enhances diagnostic precision beyond traditional methods. This innovation improves the quality of healthcare services and supports the goal of universal health coverage by providing more efficient and effective diagnostic pathways.
Conclusion: Advancing Health Equity through Technological Innovation
The AI-assisted diagnostic model developed in this study offers a robust, accurate, and clinically valuable tool for differentiating PJP from BP. Its successful validation underscores the transformative potential of integrating digital radiology and AI with clinical data to address complex diagnostic challenges. By improving diagnostic precision, this model empowers clinicians to make more confident and timely therapeutic decisions, ultimately contributing to the reduction of pneumonia-related mortality. This research marks a critical step forward in leveraging technology to achieve Sustainable Development Goal 3, ensuring better health outcomes and promoting well-being for populations worldwide.
Analysis of Sustainable Development Goals (SDGs) in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
- The article directly addresses global health issues by focusing on pneumonia, which it identifies as a “leading cause of morbidity and mortality worldwide.” The entire study is aimed at improving the diagnosis and treatment of specific pneumonia subtypes (PJP and BP) to enhance patient outcomes and reduce mortality, which is the core mission of SDG 3.
-
SDG 9: Industry, Innovation, and Infrastructure
- The research heavily relies on and promotes technological innovation and scientific research. It discusses the application of advanced technologies like “Artificial intelligence (AI),” “metagenomic next-generation sequencing (mNGS),” and “High-resolution chest CT” to solve a complex medical challenge. This focus on leveraging technology and research to upgrade healthcare capabilities aligns with SDG 9’s goal of fostering innovation.
-
SDG 17: Partnerships for the Goals
- The study exemplifies collaboration, a key principle of SDG 17. The article states it is a “retrospective, multicenter study” conducted at “two hospitals.” Furthermore, it acknowledges financial support from a university hospital grant, showcasing a partnership within the academic and healthcare sectors to advance scientific knowledge and public health.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Targets under SDG 3: Good Health and Well-being
- Target 3.3: “By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.” Pneumonia is a major communicable disease. The article’s effort to create a diagnostic model that can “enhance diagnostic accuracy, support empirical anti-infective decision-making, and improve patient prognosis” directly contributes to combating this disease.
- Target 3.4: “By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment…” The article notes that the PJP group had a significantly “higher incidence of chronic diseases (93.6% vs. 63.5%)” such as malignancies and cardiovascular diseases. By improving the diagnosis of pneumonia in this vulnerable population, the study helps reduce mortality linked to complications in patients with NCDs.
- Target 3.d: “Strengthen the capacity of all countries… for early warning, risk reduction and management of national and global health risks.” The development of an AI-based predictive model for PJP is a direct effort to strengthen the capacity for early and accurate diagnosis (early warning) and guide timely treatment, thereby managing a significant health risk.
-
Target under SDG 9: Industry, Innovation, and Infrastructure
- Target 9.5: “Enhance scientific research, upgrade the technological capabilities of industrial sectors in all countries… encouraging innovation…” The study is a clear example of enhancing scientific research. It introduces an “AI-assisted CT analysis” and a “diagnostic prediction model,” which represents an upgrade in the technological capabilities of the medical diagnostics field. The funding mentioned in the article also points to investment in research and development.
-
Target under SDG 17: Partnerships for the Goals
- Target 17.17: “Encourage and promote effective public, public-private and civil society partnerships…” The research was a collaboration between “The Second Affiliated Hospital of Fujian Medical University and Affiliated Hospital of Putian University” and was supported by a university grant. This represents an effective public-sector partnership to achieve health-related research goals.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Indicators for SDG 3 Targets
- Mortality Rate: The article explicitly provides mortality rates for the patient groups (“mortality (48.9% vs. 34.6%)”). The goal of the new diagnostic model is to improve treatment and ultimately lower these rates, making mortality a key indicator of progress.
- Diagnostic Accuracy Metrics: The study’s success is measured by several performance indicators of the AI model. These include “accuracy of 84.2% in the training cohort and 81.6% in the validation cohort,” “Area Under the Curve (AUC) of 0.898,” “specificity of 0.904, and sensitivity of 0.745.” These metrics directly quantify the improved capacity for early and accurate diagnosis (Target 3.d).
- Incidence of Chronic Disease in Patient Cohorts: The article reports a “higher incidence of chronic diseases (93.6% vs. 63.5%)” in PJP patients. Tracking outcomes for this specific sub-population serves as an indicator for progress on Target 3.4.
-
Indicators for SDG 9 Target
- Research and Development Expenditure: The article provides a direct indicator of investment in R&D by stating, “This work was supported by the Doctoral Training Matching Fund of the Second Affiliated Hospital of Fujian Medical University (Grant No. 2022BD0107).”
- Number of Researchers: While not providing a total count, the “Author contributions” section lists nine individuals involved in the research, implying the presence of a dedicated research team, which relates to the indicator of research and development workers.
-
Indicators for SDG 17 Target
- Number of Multi-Stakeholder Partnerships: The study itself is an indicator of a partnership, as it is a “multicenter study” involving two distinct hospitals. The acknowledgments section thanks staff from both institutions, reinforcing this collaboration.
4. Table of SDGs, Targets, and Indicators
| SDGs, Targets and Indicators | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being |
|
|
| SDG 9: Industry, Innovation, and Infrastructure |
|
|
| SDG 17: Partnerships for the Goals |
|
|
Source: frontiersin.org
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0