AI for Health Plans: Expanding Access while Reducing Costs – Becker’s Payer Issues
Report on Leveraging Artificial Intelligence to Advance Sustainable Development Goals in Healthcare
Introduction: Current Healthcare Challenges and Alignment with SDG 3
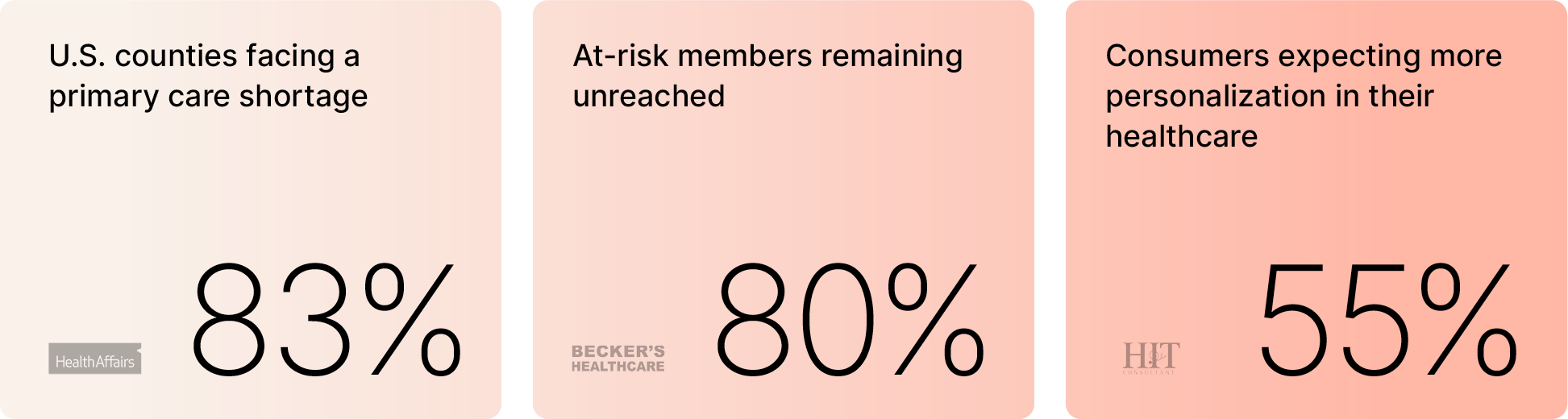
The current state of healthcare presents significant barriers to achieving Sustainable Development Goal 3 (SDG 3), which aims to ensure healthy lives and promote well-being for all at all ages. Systemic challenges in affordability, access, and patient engagement directly contravene the principles of universal health coverage (Target 3.8). An analysis of the current landscape reveals several critical issues:
- Affordability Crisis: Nearly half of the American population reports difficulty in affording basic healthcare services, creating a substantial barrier to well-being.
- Access Delays: Patients face an average wait time of 38 days to see a physician, impeding timely diagnosis and treatment.
- Engagement Gap: An estimated 80% of at-risk health plan members remain unreached by current outreach methods, leaving the most vulnerable without necessary support.
These unsustainable conditions highlight the limitations of the existing care delivery system, including constraints on clinical capacity and patient reach, necessitating innovative solutions to advance global health objectives.
The Role of AI in Achieving Universal Health Coverage (SDG 3.8)
Artificial intelligence (AI) presents a transformative opportunity to restructure the economics of care delivery and accelerate progress toward universal health coverage. Rather than replacing providers, AI serves to augment existing healthcare frameworks with intelligent systems designed to reduce costs and expand access. The primary potential lies in integrating AI technology with the rich, underleveraged data held by health plans. This synergy enables the creation of scalable systems that support key healthcare functions.
- Personalized Outreach: AI can analyze member data to deliver tailored communication and health interventions at scale.
- Intelligent Triage: Automated systems can efficiently assess patient needs and direct them to the appropriate level of care.
- Streamlined Care Navigation: AI-powered tools guide members through complex healthcare systems, ensuring they receive the right care in the right setting at the right time.
Enhancing Healthcare Infrastructure and Innovation (SDG 9)
The integration of AI into healthcare aligns with SDG 9, which calls for building resilient infrastructure and fostering innovation. By creating a sustainable and scalable omnichannel access model, health plans can meet members through various channels, including phone, online platforms, and in-home services. AI-driven asynchronous-first solutions offer a prime example of this innovation, providing 24/7 access to personalized and cost-effective care. The implementation of such technologically advanced infrastructure has yielded measurable results:
- Cost Reduction: One health plan reported $17 per member per month (PMPM) in savings within 120 days.
- Improved Health Outcomes: The same implementation saw a significant drop in hospital readmission rates.
- Enhanced Member Satisfaction: The accessibility and convenience of the new model led to a rise in overall satisfaction scores.
Reducing Health Inequalities through Automated Engagement (SDG 10)
AI-powered systems can play a crucial role in advancing SDG 10 (Reduced Inequalities) by ensuring consistent and proactive engagement with all patient populations, particularly those who are hard to reach. Automated outreach for medication reminders and post-visit follow-ups improves treatment adherence and reduces adverse outcomes. These systems consistently outperform manual outreach efforts by driving higher response rates without increasing the clinical burden on healthcare providers. This technological approach helps bridge the engagement gap and promotes more equitable health outcomes across diverse communities.
Conclusion: A Connected Care Model for Sustainable Health Outcomes
To fully realize the potential of technology in healthcare, a shift from piecemeal digitization to a fully integrated, end-to-end system is required. Unifying the care journey streamlines workflows, automates administrative tasks, and enhances overall efficiency, which directly contributes to cost reduction and improved patient experiences. This connected care model is fundamental to achieving sustainable progress in global health.
- Unified Access: Providing members with a single, seamless entry point to care services.
- Intelligent Navigation: Guiding members efficiently through their healthcare journey.
- Proactive Engagement: Maintaining contact and support throughout the care continuum.
By reimagining the member experience as a connected, personalized, and proactive ecosystem, it is possible to unlock better outcomes, stronger engagement, and lower costs, thereby making substantial contributions toward achieving SDGs 3, 9, and 10.
1. Which SDGs are addressed or connected to the issues highlighted in the article?
The article highlights several challenges within the American healthcare system and proposes technological solutions, connecting its themes to the following Sustainable Development Goals (SDGs):
-
SDG 3: Good Health and Well-being
This is the most central SDG addressed. The article’s entire focus is on improving healthcare delivery, access, affordability, and patient outcomes. It directly discusses issues like the inability to afford basic healthcare and long wait times to see a doctor, which are fundamental barriers to achieving good health and well-being.
-
SDG 9: Industry, Innovation, and Infrastructure
The article strongly advocates for leveraging innovation—specifically artificial intelligence (AI)—to overhaul the existing healthcare infrastructure. It presents AI not just as a tool but as a fundamental component to create a more efficient, scalable, and sustainable care delivery system, which aligns with the goal of upgrading industrial sectors with new technology.
-
SDG 10: Reduced Inequalities
By addressing the barriers of cost and access, the article implicitly touches upon reducing health inequalities. Issues like half of Americans struggling to afford care and the difficulty in reaching “at-risk members” disproportionately affect vulnerable and low-income populations. The proposed solutions aim to create a more equitable system where care is “always within reach” for everyone, regardless of their circumstances.
2. What specific targets under those SDGs can be identified based on the article’s content?
Based on the issues and solutions discussed, the following specific SDG targets are relevant:
-
Target 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
- Financial Risk Protection & Affordability: The article directly addresses this by stating that “nearly half of Americans struggle to afford basic healthcare.” The proposed AI solutions aim to mitigate this by reducing costs, evidenced by the claim of “$17 PMPM savings” for one health plan.
- Access to Quality Essential Health-Care Services: The challenge of an “average of 38 days to see a doctor” is a direct barrier to access. The solution of “AI-driven asynchronous-first solutions” that offer “24/7 access” is designed to overcome this. The focus on improving outcomes, as shown by “readmissions dropped, and satisfaction rose,” points to the quality of these services.
-
Target 9.5: Enhance scientific research, upgrade the technological capabilities of industrial sectors in all countries… encouraging innovation.
- Technological Upgrades and Innovation: The article is a case for upgrading the healthcare sector’s technological capabilities. It argues that the current “care delivery system has yet to fully catch up” and proposes that “Artificial intelligence is poised to fundamentally change the economics of care delivery.” This directly aligns with the target of encouraging innovation to improve industrial sectors.
-
Target 10.2: By 2030, empower and promote the social, economic and political inclusion of all, irrespective of… economic or other status.
- Inclusion in Healthcare: The article highlights a significant problem of exclusion, where “80% of at-risk members remain unreachable.” By using AI to “scale personalized outreach” and meet members “where they are,” the proposed system aims to include these hard-to-reach populations, thereby reducing inequalities in healthcare access and engagement.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
Yes, the article mentions several quantitative and qualitative indicators that can be used to measure progress:
-
Indicators for Target 3.8 (Universal Health Coverage)
- Financial Burden of Healthcare: The statistic that “nearly half of Americans struggle to afford basic healthcare” serves as a baseline indicator of financial hardship due to health costs, which is related to SDG Indicator 3.8.2. The “$17 PMPM savings” is a direct measure of progress in reducing this burden.
- Access to Healthcare Services: The “average of 38 days to see a doctor” is a clear indicator of access barriers. A reduction in this wait time would signify progress. The implementation of “24/7 access” is a measure of improved service availability.
- Healthcare Quality and Outcomes: The article implies indicators of quality through phrases like “readmissions dropped” and “satisfaction rose.” These are standard metrics for evaluating the effectiveness of healthcare services.
-
Indicators for Target 10.2 (Reduced Inequalities)
- Patient Engagement Rate: The fact that “80% of at-risk members remain unreachable” is a stark indicator of inequality in engagement. An increase in the reach and response rates among these populations, which the article claims AI systems can achieve (“driving higher response rates”), would be a key indicator of progress.
4. Create a table with three columns titled ‘SDGs, Targets and Indicators” to present the findings from analyzing the article.
| SDGs | Targets | Indicators (Mentioned or Implied in the Article) |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.8: Achieve universal health coverage, including financial risk protection and access to quality, affordable healthcare. |
|
| SDG 9: Industry, Innovation, and Infrastructure | 9.5: Enhance research and upgrade the technological capabilities of industrial sectors. |
|
| SDG 10: Reduced Inequalities | 10.2: Empower and promote the social and economic inclusion of all. |
|
Source: beckerspayer.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0