H.R. 1 Jeopardizes Californians’ Access to Behavioral Health Care and Key State Reforms – California Budget & Policy Center

Report on the Impact of Federal Legislation H.R. 1 on California’s Behavioral Health System and Sustainable Development Goals
Executive Summary
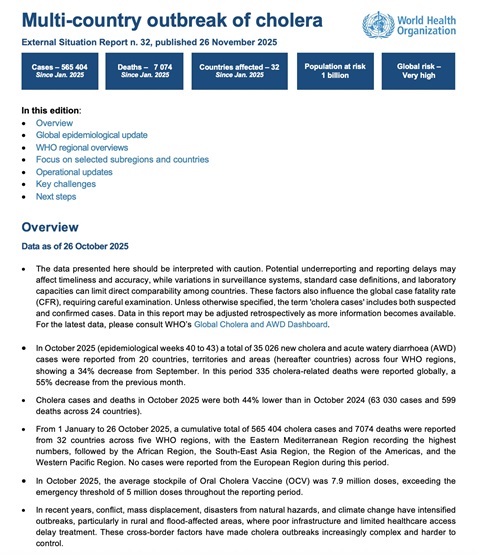
This report analyzes the implications of the recently enacted federal legislation, H.R. 1, on California’s behavioral health system. The legislation’s deep cuts to Medi-Cal (California’s Medicaid program) pose a significant threat to the state’s progress in achieving several United Nations Sustainable Development Goals (SDGs), particularly SDG 3 (Good Health and Well-being), SDG 10 (Reduced Inequalities), and SDG 11 (Sustainable Cities and Communities). By undermining the financial foundation of Medi-Cal, H.R. 1 jeopardizes access to essential mental health and substance use services for millions, disproportionately affecting vulnerable populations and reversing advancements in integrated care and housing support systems.
Medi-Cal: A Foundation for Health, Equality, and Sustainable Communities (SDGs 3, 10, 11)
California’s behavioral health system is fundamentally reliant on Medi-Cal, which serves as the primary vehicle for delivering care and advancing key SDG targets. Over one-third of Californians depend on the program for essential health services.
Alignment with SDG 3: Good Health and Well-being
Medi-Cal is critical for promoting mental health and well-being for all ages. In 2023, approximately 8.25 million Medi-Cal enrollees accessed mental health services. The program provides a lifeline for:
- Adults: Nearly one in five California adults experiences mental illness, and one in six faces a substance use disorder. Medi-Cal provides integrated care for these individuals, including the nearly 345,000 adults who received Specialty Mental Health Services in 2021-22.
- Children and Youth: Medi-Cal covers three in seven California children, funding essential services like school-based mental health support. In 2021-22, over 246,000 individuals under 21 received care through Medi-Cal Specialty Mental Health Services.
Alignment with SDG 10: Reduced Inequalities
Medi-Cal is a primary tool for reducing health disparities among marginalized groups. It provides coverage to populations that face systemic barriers to care, thereby promoting equity.
- Vulnerable Youth: The program is essential for youth of color and LGBTQ+ youth, who report high rates of stress and face compounded risks due to historical and ongoing discrimination.
- Economically Disadvantaged Populations: By providing health coverage, Medi-Cal mitigates the risk of catastrophic health expenditures, a key driver of poverty (related to SDG 1: No Poverty).
Alignment with SDG 11: Sustainable Cities and Communities
The program directly supports efforts to make communities inclusive and safe by linking healthcare with housing stability.
- Homelessness Response: Approximately 75% of Californians experiencing homelessness are covered by Medi-Cal. The program funds services that help individuals with behavioral health needs find and maintain stable housing, which is a critical component of ending homelessness.
H.R. 1: A Setback for California’s Progress on the 2030 Agenda
The enactment of H.R. 1 introduces severe cuts and restrictions that directly threaten the state’s ability to meet its SDG commitments. The legislation is projected to slash approximately $1 trillion from Medicaid nationally over the next decade, potentially causing up to 3.4 million Californians to lose coverage and costing the state up to $30 billion in federal funding annually.
Mechanisms Undermining SDG Attainment
The legislation destabilizes the behavioral health system through two primary mechanisms:
- Financing Restrictions: H.R. 1 imposes new rules that invalidate California’s Managed Care Organization (MCO) tax structure, a key mechanism for drawing down federal matching funds. This directly threatens the financial sustainability of the health system, undermining SDG 3. The loss of these funds jeopardizes investments in behavioral health facilities and workforce expansion.
- Eligibility and Access Barriers: The law introduces new administrative hurdles that will disproportionately harm vulnerable populations, directly contravening the goal of reducing inequalities (SDG 10).
Specific Restrictions and Their Impact on SDGs
- Exclusion of Immigrant Groups: Denying Medi-Cal coverage to refugees, asylees, and other immigrants with humanitarian protections exacerbates inequality and leaves a highly vulnerable population without access to essential care (violates SDG 10).
- Work Requirements: Imposing burdensome reporting requirements on adults could lead to 3 million Californians losing coverage. This creates significant barriers for individuals with behavioral health conditions and those experiencing homelessness, pushing them further into poverty and ill-health (violates SDG 1 and SDG 3).
- Increased Eligibility Checks: More frequent checks risk disrupting continuous care, which is critical for managing chronic mental health or substance use conditions, leading to poorer health outcomes (violates SDG 3).
- Limited Retroactive Coverage: Reducing the retroactive coverage period leaves individuals in crisis, such as those experiencing a psychiatric emergency or overdose, exposed to significant medical debt (violates SDG 1 and SDG 3).
Jeopardizing State Initiatives Aligned with Sustainable Development
H.R. 1 places California’s innovative, interconnected behavioral health reforms at risk. These initiatives are designed to create an equitable and coordinated system of care, embodying the principles of the SDGs.
Threats to Integrated Care Models
- CalAIM and the Behavioral Health Services Act (BHSA): These initiatives integrate health services (SDG 3) with housing supports (SDG 11) for the most vulnerable. CalAIM’s Community Supports have already delivered over 1.1 million services since 2022. The loss of Medi-Cal funding and eligibility for enrollees undermines the foundation of this model.
- BH-CONNECT: This initiative strengthens community-based care for Medi-Cal members with significant behavioral health needs, building stronger and more equitable health systems in line with SDG 16 (Peace, Justice and Strong Institutions).
- Children and Youth Behavioral Health Initiative (CYBHI): This program expands school-based prevention and early intervention services, supporting healthy development (SDG 3) and quality education (SDG 4). Cuts to Medi-Cal threaten the reimbursement streams that make these services possible.
Conclusion and Recommendations for State Action
The federal cuts mandated by H.R. 1 represent a significant regression for California’s commitment to the Sustainable Development Goals. The legislation threatens to dismantle a system that promotes good health, reduces deep-seated inequalities, and contributes to sustainable and inclusive communities. State leaders must take decisive action to mitigate this harm and protect the well-being of all Californians.
To uphold its commitment to the 2030 Agenda, it is recommended that California policymakers:
- Protect Vulnerable Populations: Implement administrative solutions to minimize disenrollment and ensure continuous access to care, upholding the principle of “leaving no one behind.”
- Secure Sustainable State-Level Funding: Explore and enact measures to raise significant, ongoing state revenue to backfill federal funding cuts and protect essential behavioral health and housing services.
- Defend Integrated Care Models: Safeguard the progress made through initiatives like CalAIM and CYBHI, which are national models for achieving integrated health, housing, and social support in line with the SDGs.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
- The article’s primary focus is on behavioral health, which includes mental health care and substance use disorder treatment. It discusses the importance of Medi-Cal in providing these essential health services to millions of Californians, including children, youth, and adults. The potential cuts to Medi-Cal under H.R. 1 directly threaten the health and well-being of the population.
-
SDG 1: No Poverty
- The article connects health care access to economic stability. It highlights that losing Medi-Cal coverage can create financial hardship, especially for those who might face catastrophic costs for psychiatric emergencies or overdose treatment. Furthermore, it discusses how Medi-Cal supports programs that help unhoused individuals, linking health care access directly to homelessness, a key dimension of poverty.
-
SDG 10: Reduced Inequalities
- The article explicitly points out the disproportionate impact of behavioral health challenges and potential service cuts on vulnerable and marginalized groups. It mentions that H.R. 1 includes “discriminatory restrictions based on age or immigration status” and specifically notes that “Black, Latinx, Native American, and Pacific Islander children and youth face the highest rates of serious emotional disturbances.” It also highlights the high rates of mental health challenges among youth of color and LGBTQ+ youth.
-
SDG 11: Sustainable Cities and Communities
- A significant theme is the link between behavioral health, housing, and homelessness. The article details how federal cuts weaken California’s homelessness response by making it harder for unhoused people to access Medi-Cal funded services. It describes state initiatives like CalAIM, which provide “housing navigation, security deposits, and transitional rent” to help people find and maintain stable housing, directly addressing the goal of adequate housing for all.
-
SDG 16: Peace, Justice and Strong Institutions
- The article analyzes the impact of a specific piece of legislation (H.R. 1) on state-level institutions and public services. It discusses how the law undermines the financial foundation of California’s behavioral health system and its key reforms (CalAIM, BH-CONNECT, etc.). This relates to the effectiveness and accountability of governmental institutions in delivering essential services and protecting citizens’ well-being.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Under SDG 3 (Good Health and Well-being):
- Target 3.4: By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being. The article’s entire focus on providing mental health care and substance use treatment through Medi-Cal directly supports this target.
- Target 3.5: Strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol. The article repeatedly mentions “substance use disorder treatment” as a core component of the behavioral health services threatened by the funding cuts.
- Target 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all. The article centers on the threat to Medi-Cal, California’s public health insurance program, which is a key mechanism for achieving universal health coverage in the state. The potential for “millions of people… to lose coverage” is a direct challenge to this target.
-
Under SDG 1 (No Poverty):
- Target 1.3: Implement nationally appropriate social protection systems and measures for all, including floors, and by 2030 achieve substantial coverage of the poor and the vulnerable. Medi-Cal is a critical social protection system discussed in the article. The threat of “3.4 million Californians” losing coverage directly impacts the state’s ability to meet this target.
-
Under SDG 10 (Reduced Inequalities):
- Target 10.2: By 2030, empower and promote the social, economic and political inclusion of all, irrespective of age, sex, disability, race, ethnicity, origin, religion or economic or other status. The article highlights how H.R. 1 would “Exclude immigrant groups from Medi-Cal coverage” and disproportionately harm people with behavioral health conditions (a disability), youth of color, and LGBTQ+ youth, undermining their inclusion in essential health systems.
- Target 10.3: Ensure equal opportunity and reduce inequalities of outcome, including by eliminating discriminatory laws, policies and practices. The article describes H.R. 1 as having “discriminatory restrictions based on age or immigration status,” which directly creates inequalities of outcome in health access.
-
Under SDG 11 (Sustainable Cities and Communities):
- Target 11.1: By 2030, ensure access for all to adequate, safe and affordable housing and basic services and upgrade slums. The article details how Medi-Cal funds programs like CalAIM that provide “housing navigation” and “transitional rent” to help unhoused individuals, directly contributing to this target. The cuts threaten these “homelessness-ending housing supports.”
-
Under SDG 16 (Peace, Justice and Strong Institutions):
- Target 16.6: Develop effective, accountable and transparent institutions at all levels. The article examines how a federal law (H.R. 1) impacts the effectiveness of state institutions and programs designed to provide behavioral health care. The potential destabilization of the entire behavioral health system due to this law is a measure of institutional ineffectiveness in protecting public services.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
For SDG 3 Targets (Health and Well-being):
- Prevalence of conditions: “Nearly 1 in 5 California adults experience some form of mental illness,” “about 1 in 20 have a serious mental illness,” and “1 in 14 children has an emotional disturbance.” These statistics serve as baseline indicators for mental health needs.
- Service utilization: “In 2023, over half of all people enrolled in Medi-Cal — roughly 8.25 million people… accessed mental health services.” Also, “nearly 345,000 adults… had at least one Medi-Cal Speciality Mental Health Services visit” in 2021-22, and “more than 246,000 [children] received care.” These numbers indicate the reach of treatment services.
- Coverage rates: “More than one in three Californians rely on Medi-Cal.” The potential loss of coverage for “as many as 3.4 million Californians” is a direct indicator for measuring progress (or regression) on universal health coverage.
-
For SDG 1 Target (Poverty):
- Coverage of social protection systems: The number of people enrolled in Medi-Cal and the potential “3.4 million Californians” who could lose coverage serve as direct indicators of the reach of this social protection system for the poor and vulnerable.
-
For SDG 10 Targets (Inequalities):
- Disaggregated data on health access: The article points to the need to track outcomes for specific groups, stating H.R. 1 “Excludes immigrant groups from Medi-Cal coverage” and that “Black, Latinx, Native American, and Pacific Islander children and youth face the highest rates of serious emotional disturbances.” Tracking coverage and service access for these specific populations would be a key indicator.
-
For SDG 11 Target (Housing):
- Number of people receiving housing support: The article states that between January and March 2025, CalAIM’s housing supports “served 68,000 adults and nearly 13,000 children experiencing homelessness.” This is a quantifiable indicator of progress in providing housing services to the homeless population.
- Health coverage among the homeless: The statistic that “roughly 75% [of unhoused Californians] were covered by Medi-Cal” is an indicator of access to basic services for this vulnerable group.
-
For SDG 16 Target (Strong Institutions):
- Public expenditure on essential services: The potential loss of “up to $30 billion in federal Medicaid funding each year” is a financial indicator of the impact on the state’s institutional capacity to provide health services.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being |
3.4 Promote mental health and well-being.
3.5 Strengthen the prevention and treatment of substance abuse. 3.8 Achieve universal health coverage. |
– Prevalence of mental illness (1 in 5 adults) and serious mental illness (1 in 20 adults). – Number of people accessing mental health services through Medi-Cal (8.25 million in 2023). – Number of adults and children receiving Medi-Cal Specialty Mental Health Services. – Proportion of the population covered by Medi-Cal (more than one in three Californians). – Number of people at risk of losing health coverage (up to 3.4 million). |
| SDG 1: No Poverty | 1.3 Implement nationally appropriate social protection systems. |
– Proportion of the population covered by social protection systems (i.e., Medi-Cal enrollment). – Number of people at risk of losing social protection coverage (3.4 million). |
| SDG 10: Reduced Inequalities |
10.2 Promote social, economic, and political inclusion of all.
10.3 Ensure equal opportunity and reduce inequalities of outcome. |
– Mention of policies that exclude specific groups (e.g., “Excludes immigrant groups from Medi-Cal coverage”). – Disproportionate rates of serious emotional disturbances among youth of color (Black, Latinx, Native American, Pacific Islander). – High rates of stress and fear of discrimination among youth of color and LGBTQ+ youth. |
| SDG 11: Sustainable Cities and Communities | 11.1 Ensure access for all to adequate, safe and affordable housing and basic services. |
– Number of homeless individuals receiving housing supports through state programs (68,000 adults and 13,000 children via CalAIM in a 3-month period). – Proportion of the homeless population with access to basic services (75% of unhoused Californians covered by Medi-Cal). |
| SDG 16: Peace, Justice and Strong Institutions | 16.6 Develop effective, accountable and transparent institutions at all levels. |
– Amount of federal funding for public health services at risk (up to $30 billion annually for California). – Impact of federal legislation (H.R. 1) on the stability and financing of state-run health and housing initiatives (CalAIM, BH-CONNECT, etc.). |
Source: calbudgetcenter.org
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0