9&10 News: Rising insurance rates threaten healthcare access in Northern Michigan – Michigan Health & Hospital Association

Report on Impending Healthcare Challenges in Michigan and Implications for Sustainable Development Goals
Introduction: Projected Insurance Rate Increases
- A projected 20% average increase in Michigan’s Affordable Care Act (ACA) marketplace insurance rates is anticipated for 2026.
- This development poses a significant challenge to the state’s progress towards the Sustainable Development Goals (SDGs), particularly by threatening the stability of the healthcare system in rural regions.
Direct Impact on SDG 3: Good Health and Well-being
- Threats to Universal Health Coverage: Rising premiums are expected to cause a decline in insurance enrollment as individuals forgo coverage due to affordability issues. This directly undermines the objective of achieving universal health coverage, a key target of SDG 3.
- Deterioration of Health Outcomes: Uninsured or underinsured individuals often delay necessary medical treatment. This can lead to manageable health issues escalating into more severe and costly conditions, compromising long-term health and quality of life, contrary to the goals of SDG 3.
- Unsustainable Pressure on Emergency Services: Delayed care frequently results in increased utilization of emergency departments for conditions that could be managed in primary care settings. This is an inefficient and unsustainable model for healthcare delivery that is detrimental to achieving SDG 3.
- Compromised Healthcare System Stability: The anticipated changes threaten an already fragile healthcare ecosystem. A shrinking and sicker insurance risk pool, as healthier individuals opt out of coverage, places financial strain on both insurers and providers, jeopardizing the infrastructure needed to ensure good health for all.
Socio-Economic Consequences and Alignment with Broader SDGs
- SDG 1 (No Poverty) & SDG 10 (Reduced Inequalities): The inability to afford health insurance or pay for medical services can push individuals and families into financial hardship, directly conflicting with SDG 1. These challenges are likely to disproportionately affect rural and low-income populations, exacerbating existing health and economic disparities and hindering progress on SDG 10.
- SDG 8 (Decent Work and Economic Growth): Financial instability among healthcare providers, resulting from uncompensated care, threatens the viability of medical facilities. This could impact employment in the healthcare sector and negatively affect the broader economy, as a healthy populace is fundamental to a productive workforce and sustainable economic growth.
Expert Analysis and Outlook
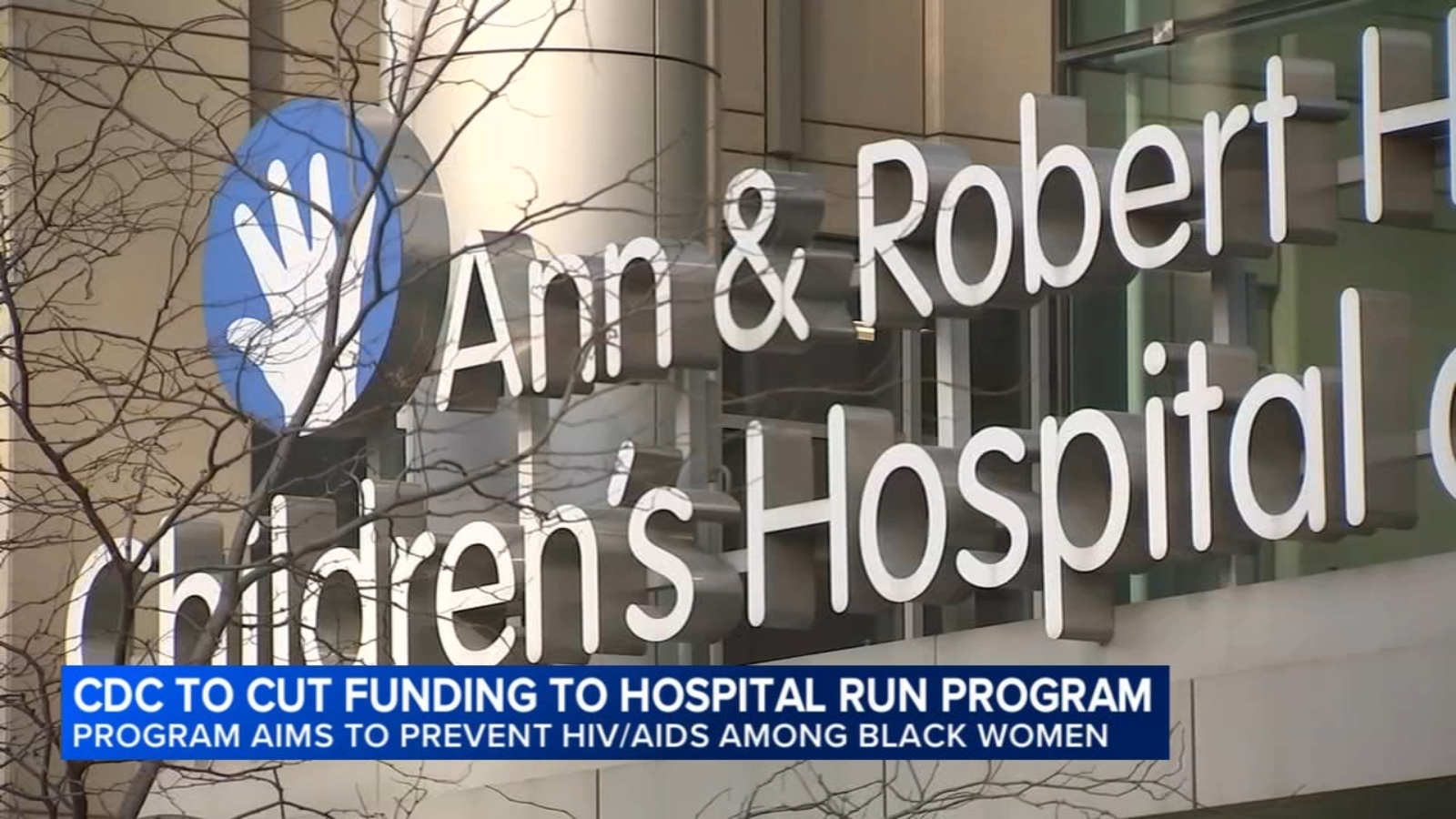
- Brian Peters, CEO, Michigan Health and Hospital Association: Emphasized the fragility of the state’s healthcare ecosystem and warned against inflicting further damage that would impede progress toward SDG 3.
- Margaret Anderson, President, Health Alliance Plan: Noted that as healthier individuals drop coverage, the remaining insurance risk pool will consist of sicker individuals who utilize more services, driving costs up and making affordable coverage even less attainable.
- Bret Jackson, President, Michigan Health Purchasers Coalition: Expressed concern that rising rates will lead to more uninsured residents, creating a cycle of financial strain for both patients and providers that undermines both SDG 1 and SDG 3.
- Jeremy Cannon, Chief Nursing Officer, Kalkaska Memorial Hospital: Highlighted that delays in treatment lead to increased use of emergency departments, which is not a sustainable long-term solution and is detrimental to individual health and well-being.
Conclusion: A Challenge to Sustainable Development
The projected increase in health insurance premiums in Michigan presents a multi-faceted challenge to sustainable development. It directly threatens the achievement of SDG 3 (Good Health and Well-being) by creating barriers to universal health coverage and promoting negative health outcomes. The cascading economic effects also jeopardize progress toward SDG 1 (No Poverty), SDG 10 (Reduced Inequalities), and SDG 8 (Decent Work and Economic Growth). Addressing this issue is critical to maintaining a sustainable and equitable healthcare system for all residents of the state.
1. Which SDGs are addressed or connected to the issues highlighted in the article?
SDG 3: Good Health and Well-being
- The article directly addresses this goal by focusing on the challenges to Michigan’s healthcare system. It discusses how rising health insurance costs threaten access to care, which can lead to “worse health outcomes.” The entire discussion revolves around ensuring people can maintain their health without financial hardship.
SDG 1: No Poverty
- This goal is connected through the theme of financial hardship caused by healthcare costs. The article states that when people cannot afford insurance, they “struggle to pay their bills.” This financial strain is a significant driver of poverty and economic instability for individuals and families.
SDG 10: Reduced Inequalities
- The article touches on this goal by highlighting the vulnerability of specific areas, noting that the healthcare industry is “already struggling in rural areas.” This implies that the negative effects of rising insurance costs will not be felt equally, potentially worsening the gap in healthcare access and quality between different geographic and economic groups.
2. What specific targets under those SDGs can be identified based on the article’s content?
SDG 3: Good Health and Well-being
-
Target 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
- The article’s core concern is the erosion of health coverage due to affordability. The statement that a 20% rate increase will likely cause “some forgo purchasing coverage” and become “uninsured” directly relates to the challenge of achieving universal health coverage and protecting citizens from financial risk associated with healthcare.
SDG 1: No Poverty
-
Target 1.3: Implement nationally appropriate social protection systems and measures for all, including floors, and by 2030 achieve substantial coverage of the poor and the vulnerable.
- The article discusses key social protection systems like the Affordable Care Act (ACA) marketplace, Medicaid, and Medicare. The concerns about “looming increases in health insurance rates” and potential “cuts to Medicaid” point to a weakening of these systems, which are designed to provide a financial safety net and ensure healthcare access for vulnerable populations.
SDG 10: Reduced Inequalities
-
Target 10.4: Adopt policies, especially fiscal, wage and social protection policies, and progressively achieve greater equality.
- The article analyzes the real-world impact of social protection policies (or the lack thereof, such as expiring subsidies). It demonstrates how changes in these policies can lead to greater inequality, as rising costs create barriers to care that disproportionately affect those with lower incomes and those in already underserved rural areas.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
SDG 3: Good Health and Well-being
- Indicator 3.8.1 (Coverage of essential health services): This is implied by the prediction of “lower enrollment” and the concern that people will “go without and be uninsured.” A decrease in the number of people with health insurance is a direct measure of reduced coverage.
- Indicator 3.8.2 (Proportion of population with large household expenditures on health): This is strongly implied by the statement that uninsured individuals will “struggle to pay their bills” for medical services. This points to an increase in out-of-pocket spending and financial hardship due to healthcare costs.
SDG 1: No Poverty
- Indicator 1.3.1 (Proportion of population covered by social protection floors/systems): The article suggests this indicator will worsen. The expected “lower enrollment” in the ACA marketplace due to rising premiums directly translates to a lower proportion of the population being covered by this specific social protection system.
SDG 10: Reduced Inequalities
- Disparity in health insurance coverage between rural and urban populations: While not a formal UN indicator, the article implies its relevance by stating the healthcare ecosystem is “already struggling in rural areas.” An increase in the uninsured rate that is more pronounced in these areas would be a key indicator of rising inequality.
4. Create a table with three columns titled ‘SDGs, Targets and Indicators” to present the findings from analyzing the article.
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.8: Achieve universal health coverage, including financial risk protection and access to quality essential health-care services. |
|
| SDG 1: No Poverty | 1.3: Implement nationally appropriate social protection systems and achieve substantial coverage of the poor and vulnerable. |
|
| SDG 10: Reduced Inequalities | 10.4: Adopt policies, especially social protection policies, and progressively achieve greater equality. |
|
Source: 9and10news.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0