Dynamics of multimorbidity patterns in older population across socioeconomic areas – Nature
Report on the Dynamics of Multimorbidity Patterns and Their Link to Socioeconomic Status and Sustainable Development Goals
1.0 Executive Summary
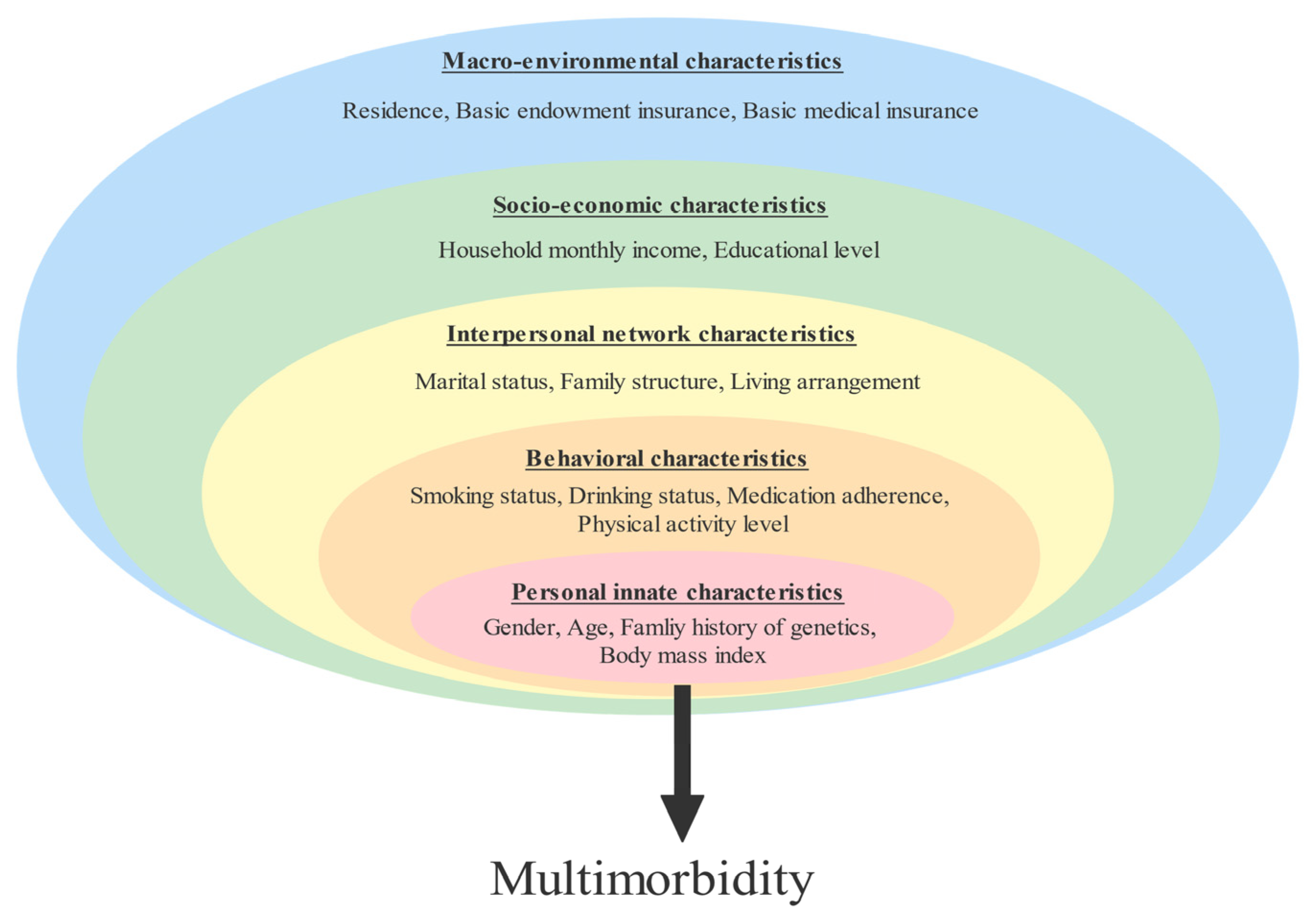
This report details a longitudinal study analyzing the evolution of multimorbidity (the presence of two or more chronic diseases) and its association with socioeconomic conditions. The findings provide critical evidence for public health policy, particularly in the context of achieving the United Nations Sustainable Development Goals (SDGs). The analysis reveals that socioeconomic disadvantage significantly accelerates the progression to complex and severe disease patterns, undermining progress towards SDG 3 (Good Health and Well-being) and exacerbating challenges related to SDG 10 (Reduced Inequalities). Key gender-specific drivers were identified, highlighting the need for targeted interventions to advance SDG 5 (Gender Equality) in health.
2.0 Introduction: Multimorbidity as a Barrier to Sustainable Development
The increasing prevalence of multimorbidity presents a formidable challenge to global health systems and sustainable development. The co-occurrence of multiple chronic conditions is linked to reduced quality of life, increased healthcare costs, and functional decline, directly impeding the achievement of SDG 3, which aims to ensure healthy lives and promote well-being for all at all ages. Furthermore, evidence suggests that the burden of multimorbidity is not distributed equally, with socioeconomic factors playing a crucial role. This study addresses this gap by examining the dynamic trajectories of disease patterns over time and their relationship with socioeconomic gradients, providing insights essential for crafting policies that promote health equity as envisioned in SDG 10.
3.0 Methodological Framework
3.1 Study Design and Population
An observational, longitudinal study was conducted using anonymized health records from the Population Health Database of the Andalusian Health Service in Southern Spain. The study cohort comprised 341,343 individuals aged 50 and over, with data collected over a ten-year period from 2011 to 2021. This large-scale, long-term approach allows for a robust analysis of disease progression and its determinants.
3.2 Data Analysis and Socioeconomic Metrics
The analytical approach was structured to identify and track changes in health status over time and link them to social determinants of health.
- Identification of Baseline Patterns: Latent Class Analysis (LCA) was used to establish initial multimorbidity patterns for the year 2011.
- Analysis of Disease Trajectories: Hidden Markov Models (HMM) were employed to probabilistically model the evolution of these patterns over the ten-year study period, identifying transitions from initial disease states to more complex, multisystemic profiles.
- Socioeconomic Stratification: Residential areas were categorized into low, medium, and high socioeconomic status (SES) based on a Deprivation Index and per capita income. This stratification allows for a direct assessment of how inequality, a central concern of SDG 10, impacts health trajectories.
4.0 Key Findings: The Socioeconomic Gradient in Chronic Disease Progression
4.1 Dynamics and Transitions of Multimorbidity Patterns
The analysis identified several distinct multimorbidity patterns and their evolution. A significant portion of the population transitioned from a state of low multimorbidity to more defined and complex disease profiles over the decade.
- Initial States: In 2011, a large proportion of individuals, particularly in the younger cohort (50-64 years), were classified in a “Not or low multimorbidity” pattern.
- Progression Pathways: Over time, these individuals transitioned towards specific disease patterns. The progression to “Complex” multimorbidity (involving three or more organ systems) was a critical finding, representing a significant decline in health status.
- Gender-Specific Drivers: The pathways to complex multimorbidity differed significantly by gender, a key consideration for SDG 5 (Gender Equality).
- For women, mental health patterns (anxiety, depression) were a primary driver towards complex physical health profiles.
- For men, patterns involving substance use disorders and related liver diseases were prominent and associated with worsening health.
4.2 Multimorbidity Disparities by Socioeconomic Area
A clear socioeconomic gradient was observed in the prevalence and progression of multimorbidity patterns, directly illustrating the challenge of SDG 10 (Reduced Inequalities).
- Individuals residing in low-SES areas developed more complex and severe combinations of diseases at an earlier age compared to those in high-SES areas.
- In the 65-79 age group, the “Complex” and “Diabetes + Hypertension” patterns were significantly more prevalent in low-SES areas.
- Conversely, the “Not or low Multimorbidity” pattern was more common in high-SES areas, indicating that populations in more affluent areas maintain better health for longer.
- The pattern of “Dependences + Liver disease + Mental” issues in men was significantly more frequent in low-SES areas, highlighting a concentration of high-risk health profiles in disadvantaged communities.
5.0 Discussion and Conclusions: Policy Implications for the SDGs
5.1 Health Inequity as a Determinant of Disease Trajectories
This study provides robust longitudinal evidence that socioeconomic status is a powerful determinant of chronic disease progression. The premature development of complex multimorbidity in disadvantaged populations represents a significant barrier to achieving SDG 3 (Good Health and Well-being) and demonstrates a clear failure to meet the objectives of SDG 10 (Reduced Inequalities). The findings suggest that policies must move beyond a purely clinical focus to address the underlying social determinants of health.
5.2 Recommendations for SDG-Aligned Health Interventions
The results of this report support the development of targeted policies aimed at preventing and controlling multimorbidity, with a focus on health equity.
- Promote Health Equity (SDG 10 & SDG 3): Public health strategies should prioritize disadvantaged areas with interventions aimed at preventing the onset of chronic diseases. This includes addressing risk factors associated with patterns like diabetes and hypertension, which are precursors to complex multimorbidity in low-SES populations.
- Integrate Mental and Physical Health Services (SDG 3): Given that mental health issues in women are a key driver of complex physical illness, health systems must integrate mental and physical healthcare to prevent this progression.
- Implement Gender-Responsive Health Policies (SDG 5): The distinct disease trajectories for men and women necessitate gender-sensitive prevention strategies. This includes targeted programs for substance use disorders in men and mental health support for women, particularly in low-SES communities.
- Strengthen Early Prevention (SDG 3): The study highlights the importance of early intervention. Policies should focus on preventing the transition from initial or single-system disease patterns to complex, multisystemic profiles, which carry a worse prognosis and higher cost to health systems and society.
Analysis of Sustainable Development Goals (SDGs) in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
The article is fundamentally centered on health outcomes, specifically the prevalence, evolution, and management of multimorbidity (the presence of multiple chronic diseases). It directly addresses issues of non-communicable diseases (cardiovascular, metabolic, respiratory), mental health, and substance abuse, all of which are core components of SDG 3. The study’s goal to inform policies for prevention and control of multimorbidity aligns with the overarching aim of ensuring healthy lives and promoting well-being for all at all ages.
-
SDG 10: Reduced Inequalities
A primary focus of the research is the “significant associations between multimorbidity patterns and the socioeconomic gradient of residential areas.” The study demonstrates that individuals in poorer areas experience more severe and complex disease combinations earlier in life. This directly addresses the issue of health inequalities driven by socioeconomic status, which is a key concern of SDG 10. The analysis stratifies the population by socioeconomic status (Low, Medium, and High SES) to highlight these disparities.
-
SDG 5: Gender Equality
The article consistently analyzes and reports findings disaggregated by sex, revealing significant gender-based differences in health patterns. For example, it notes that “mental health problems in women and substance use disorder related diseases in men were key drivers of worsening health.” By identifying these distinct health trajectories, the study underscores the need for gender-sensitive health policies and interventions, which is relevant to achieving gender equality in health outcomes.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Target 3.4: Reduce premature mortality from non-communicable diseases and promote mental health
The article’s entire scope is on understanding the trajectories of chronic, non-communicable diseases (NCDs) such as cardiovascular conditions, diabetes, and respiratory illnesses. It also places a strong emphasis on mental health, identifying a “Mental” pattern that is particularly prevalent in women and a key driver towards more complex health issues. The conclusion explicitly states that the research can “serve as a basis for… policies and strategies for the prevention and control of multimorbidity from an early age,” directly supporting the prevention and treatment goals of Target 3.4.
-
Target 3.5: Strengthen the prevention and treatment of substance abuse
The study identifies a specific and persistent multimorbidity pattern in men characterized by “substance use disorders or dependences (drugs, alcohol, or tobacco), mixed with liver diseases and HIV.” This finding directly relates to the need to address substance abuse and its severe health consequences, aligning with the objective of Target 3.5.
-
Target 10.2: Promote social, economic and political inclusion of all, irrespective of age, sex… or economic or other status
The research provides clear evidence of health exclusion based on economic status. The finding that “people in poorer areas often developed more complex and severe disease combinations earlier in life” highlights a significant health inequality. By analyzing how socioeconomic status impacts health trajectories, the study provides a basis for policies aimed at reducing these disparities and promoting more equitable health outcomes for all, which is the essence of Target 10.2.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Prevalence of specific multimorbidity patterns
The article identifies and quantifies the prevalence of various disease patterns (e.g., “Musculoskeletal,” “Mental,” “Cardiometabolic,” “Complex,” “Dependences + Liver disease”). These prevalence rates, when tracked over time and disaggregated by age, sex, and socioeconomic status, serve as direct indicators for monitoring the burden of NCDs and mental health conditions (relevant to Target 3.4) and substance abuse (Target 3.5).
-
Rate of transition to complex multimorbidity
The study uses Hidden Markov Models to calculate the probability of transitioning from a less severe disease pattern to a “Complex” or multisystemic one. For instance, it notes a “23% probability” for women in the “Mental” pattern to transition to the “Complex” state. This transition rate is a powerful indicator of worsening health and can be used to measure the effectiveness of preventive interventions aimed at halting disease progression.
-
Disparities in health patterns across socioeconomic areas
The article measures the differences in the prevalence of specific patterns between Low, Medium, and High SES areas. It finds, for example, that “‘Complex’ and ‘Diabetes + Hypertension’ patterns are more prevalent in Low SES areas” among women aged 65-79. The magnitude of this difference is a key indicator for tracking progress on reducing health inequalities (Target 10.2). A reduction in the gap between SES areas over time would indicate progress.
-
Gender-disaggregated prevalence of health patterns
The study’s methodology of separating analyses for men and women provides gender-specific indicators. The higher prevalence of the “Mental” pattern in women and the “Dependences” pattern in men are clear, measurable indicators. Tracking these gender-specific rates helps assess whether health systems are adequately addressing the distinct needs of men and women, contributing to the goals of SDG 5.
4. Summary Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | Target 3.4: Reduce premature mortality from non-communicable diseases (NCDs) and promote mental health. |
|
| Target 3.5: Strengthen the prevention and treatment of substance abuse. |
|
|
| SDG 10: Reduced Inequalities | Target 10.2: Promote social and economic inclusion of all, irrespective of economic or other status. |
|
| SDG 5: Gender Equality | Target 5.1: End all forms of discrimination against all women and girls everywhere. Target 5.c: Adopt and strengthen sound policies for the promotion of gender equality. |
|
Source: nature.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0