Health costs associated with pregnancy, childbirth, and infant care – healthsystemtracker.org
Report on the Financial Implications of Maternal and Infant Healthcare in the Context of Sustainable Development Goals
This report analyzes the healthcare costs associated with pregnancy, childbirth, and infancy for individuals with employer-sponsored insurance from 2021 to 2023. The findings highlight significant financial barriers that challenge the achievement of several Sustainable Development Goals (SDGs), particularly SDG 3 (Good Health and Well-being), SDG 1 (No Poverty), SDG 5 (Gender Equality), and SDG 10 (Reduced Inequalities).
Section 1: Maternal Healthcare Costs and Financial Risk Protection (SDG 3, SDG 1)
The high cost of maternal care represents a substantial obstacle to achieving universal health coverage and financial risk protection, as outlined in SDG Target 3.8. These expenses can lead to significant financial hardship, undermining efforts to eradicate poverty (SDG 1).
1.1. Aggregate Costs of Pregnancy and Childbirth
An analysis of health spending reveals that pregnancy, delivery, and postpartum care create a considerable financial burden on families, directly impacting their economic stability.
- Average Additional Health Cost for Pregnant Women: $20,416
- Average Amount Paid by Insurance: $17,674
- Average Out-of-Pocket Cost Paid by Enrollee: $2,743
These out-of-pocket costs are unaffordable for many households, with estimates showing that one-third of multi-person households and half of single-person households lack the liquid assets to cover such expenses. This financial strain increases the risk of medical debt, pushing families closer to poverty.
1.2. Cost Disparities by Delivery Type
The method of delivery significantly influences total and out-of-pocket costs, creating further financial variables for expectant families.
- Vaginal Delivery:
- Average Total Cost: $15,712
- Average Out-of-Pocket Cost: $2,563
- Cesarean Section (C-section) Delivery:
- Average Total Cost: $28,998 (85% higher than vaginal delivery)
- Average Out-of-Pocket Cost: $3,071 (20% higher than vaginal delivery)
The substantial cost for a C-section, which accounts for nearly one-third of all deliveries, underscores the need for health systems to manage costs while ensuring access to necessary medical interventions, a core component of SDG 3.
Section 2: Infant Healthcare Costs and Child Well-being (SDG 3)
Ensuring a healthy start to life is fundamental to SDG Target 3.2, which aims to end preventable deaths of newborns and children under five. However, the high cost of infant care, especially for those requiring intensive medical intervention, poses a significant challenge.
2.1. Healthcare Spending in Early Childhood
Medical costs for infants and toddlers add to the financial burden on new families.
- Newborns (0-3 months): Average total spending of $5,820, with $475 in out-of-pocket costs.
- Toddlers (18-24 months): Cumulative average total spending of $16,575, with $1,511 in out-of-pocket costs.
2.2. Impact of Neonatal Intensive Care Unit (NICU) Admission
The need for specialized neonatal care drastically increases healthcare expenditures, highlighting inequalities in health outcomes and financial impact.
- Children without NICU Admission (by 18-24 months):
- Average Total Cost: $14,268
- Average Out-of-Pocket Cost: $1,724
- Children with NICU Admission (by 18-24 months):
- Average Total Cost: $77,992
- Average Out-of-Pocket Cost: $3,021
- Children with Highest-Level NICU (Level IV) Admission: Average total cost reaches $117,878.
The five-fold increase in costs for children admitted to the NICU demonstrates the critical need for affordable, high-quality neonatal care to support child survival and well-being without causing catastrophic health expenditure for families.
Section 3: Socioeconomic Consequences and Inequality (SDG 5, SDG 10)
The financial burden of childbirth and infant care disproportionately affects women and can exacerbate existing socioeconomic inequalities, hindering progress on SDG 5 (Gender Equality) and SDG 10 (Reduced Inequalities).
3.1. Medical Debt and Gender Inequality
The high out-of-pocket costs associated with maternal care are a direct contributor to medical debt among women, impacting their economic empowerment and financial independence.
- New mothers are twice as likely to hold medical debt compared to women of the same age who have not recently given birth.
- Among women aged 18-35, 14.3% of those who gave birth in the last 18 months had medical debt over $250, compared to only 7.6% of women who did not.
This disparity underscores how healthcare costs can entrench gender-based economic inequality, making it a critical issue for SDG 5.
3.2. Systemic Barriers to Health Equity
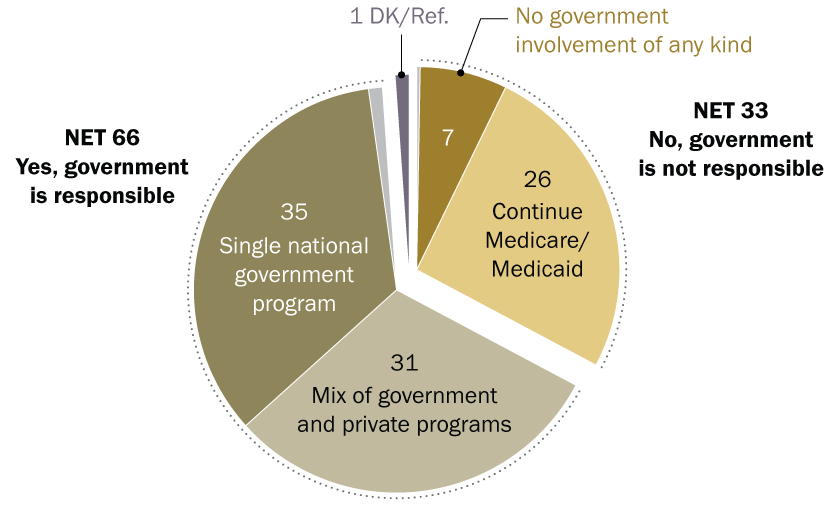
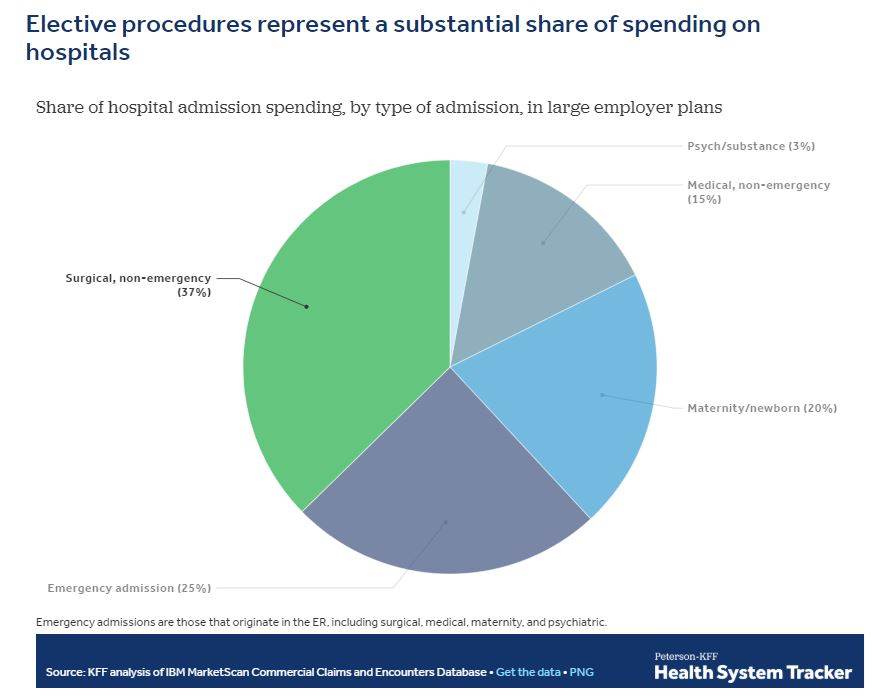
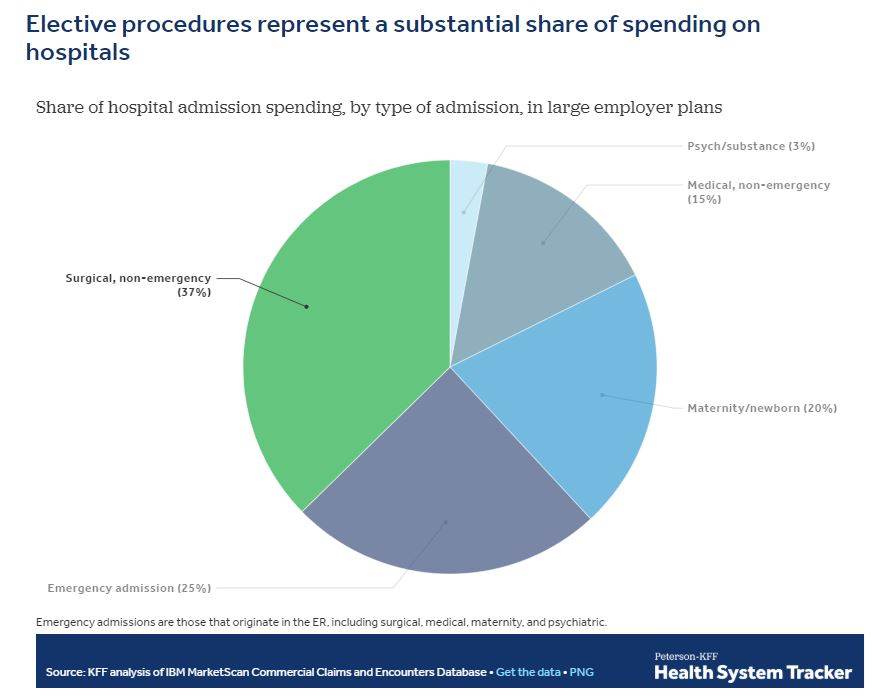
The analysis reveals systemic issues that challenge the goal of reducing inequalities (SDG 10). While half of births are covered by private insurance, the other half are covered by Medicaid, which typically involves minimal out-of-pocket costs. This creates a two-tiered system where financial burden is heavily dependent on insurance type, which is often linked to income and employment status. Addressing these high costs within private insurance is essential for creating a more equitable healthcare system for all mothers and children.
Analysis of Sustainable Development Goals (SDGs) in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
This is the most central SDG addressed. The article is entirely focused on the costs of healthcare services related to pregnancy, childbirth, postpartum, and infant care. It examines the financial aspects of accessing essential health services for mothers and newborns, which is a core component of ensuring healthy lives and promoting well-being for all at all ages.
-
SDG 1: No Poverty
The article connects high healthcare costs directly to financial hardship, which is a key driver of poverty. It states that “roughly one third of multi-person households and half of single-person households lack the liquid assets necessary to cover typical out-of-pocket costs” and that “New mothers are twice as likely to have medical debt.” This financial burden can push families into poverty or prevent them from escaping it.
-
SDG 10: Reduced Inequalities
The article highlights financial inequalities in accessing healthcare. The significant out-of-pocket expenses create a substantial barrier for families with fewer financial resources, leading to unequal financial burdens. The discrepancy in costs between vaginal ($15,712) and cesarean ($28,998) deliveries, and especially for infants requiring NICU care, shows how health status can exacerbate economic inequality.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Target 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services…
The article directly addresses this target by analyzing the high costs and significant out-of-pocket expenses associated with maternal and infant care for those with employer-sponsored insurance. The average out-of-pocket cost of $2,743 for pregnancy and the resulting medical debt demonstrate a lack of complete “financial risk protection” for families, even when they are insured.
-
Target 3.1: By 2030, reduce the global maternal mortality ratio…
While the article does not discuss mortality rates, it focuses on the costs of essential maternal health services (prenatal, delivery, postpartum care). High costs can be a barrier to accessing timely and quality care, which is a critical factor in preventing maternal mortality. The analysis of costs for different delivery types (vaginal vs. cesarean) is relevant to monitoring the quality and appropriateness of maternal healthcare.
-
Target 3.2: By 2030, end preventable deaths of newborns and children under 5 years of age…
The article details the substantial costs of infant care, particularly for newborns admitted to the Neonatal Intensive Care Unit (NICU). It notes that children admitted to the NICU “accumulate 5 times more in healthcare costs.” Ensuring financial access to this critical care is essential for reducing neonatal mortality and ending preventable deaths of newborns.
-
Target 1.3: Implement nationally appropriate social protection systems and measures for all…
The analysis of employer-sponsored health insurance functions as a case study of a social protection system. The findings, which show that many families cannot afford the out-of-pocket costs and subsequently incur medical debt, suggest that this system provides inadequate financial protection for the significant life event of childbirth.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Indicator 3.8.2: Proportion of population with large household expenditures on health as a share of total household expenditure or income.
The article provides direct data for this indicator. It quantifies the average out-of-pocket health expenditure for pregnancy ($2,743), childbirth (vaginal: $2,563; C-section: $3,071), and infant care. It further states that “New mothers are twice as likely to have medical debt,” which is a direct consequence of large health expenditures relative to a household’s ability to pay.
-
Cesarean section rate.
The article explicitly mentions this indicator, stating that “About a third of all deliveries in the United States are by caesarean (32.3% in 2023).” This is a key indicator used globally to monitor access to and appropriate use of essential maternal health services.
-
Proportion of newborns admitted to the NICU.
The article provides a figure for this indicator, noting that “nearly ten percent of newborns are admitted to the NICU.” This data point helps measure the prevalence of high-risk newborns requiring specialized, high-cost care, which is relevant to both health outcomes (Target 3.2) and financial protection (Target 3.8).
-
Average cost of health services.
The article provides detailed cost breakdowns for various services, such as the total average cost of pregnancy ($20,416), vaginal delivery ($15,712), C-section ($28,998), and infant care with a NICU stay ($77,992). These figures serve as indicators of the financial burden placed on the healthcare system and on families, which is crucial for assessing financial risk protection.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being |
|
|
| SDG 1: No Poverty |
|
|
| SDG 10: Reduced Inequalities |
|
|
Source: healthsystemtracker.org
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0