Persistence of Antiretroviral Therapy in HIV Adults – Bioengineer.org
Report on Antiretroviral Therapy Persistence and its Alignment with Sustainable Development Goals
Advancing SDG 3: Good Health and Well-being
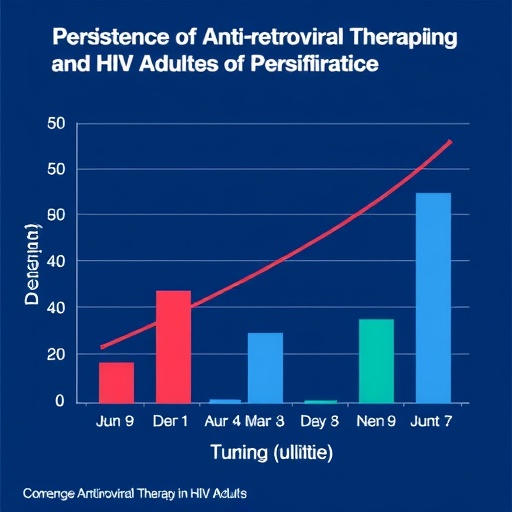
A study by Kong, A.M. et al. investigates the persistence of Antiretroviral Therapy (ART) among adults with HIV in the United States, particularly those with co-occurring mental health or substance use disorders. The findings directly inform strategies for achieving Sustainable Development Goal 3 (Good Health and Well-being), specifically its targets on ending the AIDS epidemic and promoting mental health.
- Target 3.3 (End the AIDS Epidemic): The research underscores that successful management of the HIV epidemic is critically dependent on consistent adherence to ART. Non-adherence among vulnerable populations presents a significant barrier to achieving this target.
- Target 3.4 (Promote Mental Health): The study highlights a high prevalence of mental health disorders, such as depression and anxiety, among individuals with HIV. These conditions directly impede ART adherence, creating a cycle of deteriorating physical and mental health. This emphasizes the need to integrate mental health support into standard HIV care.
- Target 3.5 (Strengthen Substance Abuse Treatment): Substance use disorders (SUD) are identified as a major complicating factor. SUD interferes with a patient’s ability to maintain treatment schedules, thereby undermining progress towards controlling the HIV epidemic. The report calls for concurrent treatment of SUD and HIV.
Addressing Socio-Economic Barriers in line with SDG 1 and SDG 10
The research illuminates how socio-economic factors create significant obstacles to treatment adherence, linking the health outcomes of individuals with HIV to broader development goals concerning poverty and inequality.
- SDG 1 (No Poverty): Financial constraints are a primary barrier, limiting access to consistent healthcare, medication, and supportive services. Addressing the economic vulnerabilities of people living with HIV is essential for ensuring uninterrupted treatment.
- SDG 10 (Reduced Inequalities): The study reveals that individuals with HIV, especially those with co-morbidities, face systemic inequalities. Barriers such as inadequate transportation, lack of social support, and limited access to specialized care disproportionately affect this population, hindering their right to health and well-being.
Policy Implications and the Role of SDG 17: Partnerships for the Goals
The findings advocate for a paradigm shift in public health policy and healthcare delivery, emphasizing integrated systems and collaborative efforts as outlined in SDG 17 (Partnerships for the Goals).
- Integrated Healthcare Models: The report strongly recommends the integration of mental health and substance abuse treatment into standard HIV care protocols. This requires a holistic approach that addresses the patient’s comprehensive needs rather than treating conditions in isolation.
- Enhanced Provider Training: To effectively manage patients with co-existing conditions, healthcare professionals require specialized training. Building capacity within the healthcare workforce is crucial for delivering effective, integrated care.
- Strengthening Support Systems: The study validates the effectiveness of support structures like peer groups and counseling services. Fostering partnerships between clinical providers and community-based support organizations is essential for promoting treatment persistence and improving quality of life.
Analysis of Sustainable Development Goals (SDGs) in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
This is the primary SDG addressed in the article. The text focuses extensively on the management of HIV, a major global health issue. It delves into the complexities of treating HIV when co-occurring with mental health disorders and substance use disorders (SUDs). The article’s core theme is improving health outcomes and ensuring well-being for individuals living with HIV by promoting adherence to antiretroviral therapy (ART) and advocating for integrated healthcare that addresses physical health, mental health, and substance abuse.
-
SDG 10: Reduced Inequalities
The article implicitly addresses SDG 10 by highlighting the unique vulnerabilities and challenges faced by a specific subgroup of the population: individuals with HIV who also struggle with mental health or substance use issues. It points out that socio-economic factors, such as financial constraints and limited access to resources, create significant barriers to treatment adherence. By calling for integrated care and support systems, the article advocates for reducing the health inequalities experienced by this marginalized group, ensuring they have an equal opportunity to achieve good health outcomes.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Target 3.3: End the epidemics of AIDS
The article directly contributes to this target by focusing on the critical factor of “persistence” and “adherence” to antiretroviral therapy (ART). The text states, “the successful treatment of HIV is not solely reliant on the efficacy of these medications; adherence to prescribed therapies remains critical.” Ending the AIDS epidemic is contingent on effective, long-term management of HIV through consistent treatment, which prevents transmission and improves the health of those living with the virus. The research highlights the barriers to this consistency, particularly in populations with co-morbidities.
-
Target 3.4: Promote mental health and well-being
This target is central to the article’s analysis. The research explicitly investigates how mental health disorders, such as “depression and anxiety,” negatively impact HIV treatment. It notes that “When mental health deteriorates, the likelihood of adhering to ART diminishes.” The article strongly advocates for integrating mental health services into standard HIV care, arguing that addressing these challenges is essential for the holistic well-being and successful medical treatment of patients.
-
Target 3.5: Strengthen the prevention and treatment of substance abuse
The article identifies substance use disorder (SUD) as a major obstacle to HIV management. It “underscores that the use of substances often interferes with a person’s capacity to maintain regular healthcare appointments, including adherence to ART.” The research calls for healthcare systems to “incorporate… substance abuse treatment into standard HIV care protocols,” directly aligning with the goal of strengthening treatment for substance abuse to improve overall health outcomes.
-
Target 3.8: Achieve universal health coverage
The article touches upon this target by discussing the “socio-economic factors affecting adherence rates.” It mentions that “Access to healthcare resources is often limited by financial constraints, transportation issues, and inadequate social support.” By highlighting these barriers, the article underscores the need for a more comprehensive and accessible healthcare system—a key component of universal health coverage—that provides not just medication but also the necessary “peer support groups, counseling services, and access to mental health professionals” to ensure everyone can maintain their treatment.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Indicator: Antiretroviral Therapy (ART) Adherence/Persistence Rates
The entire study is centered on “real-world persistence” in adults with HIV after restarting ART. This is the most direct indicator mentioned. Measuring the rate at which patients, particularly those with co-occurring mental health or substance use disorders, continue their prescribed treatment regimen is a clear metric for assessing the effectiveness of healthcare interventions and support systems.
-
Indicator: Prevalence of Co-occurring Mental Health and Substance Use Disorders in People with HIV
The article highlights that mental health disorders are “not uncommon” and that substance use is a “critical element” compounding challenges. Tracking the prevalence of these co-morbidities within the HIV-positive population would be an essential indicator to understand the scale of the problem and to target resources and integrated care models effectively.
-
Indicator: Availability of Integrated Healthcare Services
The article’s conclusion advocates for a “paradigm shift” towards “integrated healthcare” that combines medical, psychological, and social support. An implied indicator of progress would be the number or percentage of HIV care facilities that offer comprehensive services, including mental health counseling and substance abuse treatment, as part of their standard care protocols.
-
Indicator: Level of Healthcare Provider Training
The article “emphasizes that healthcare professionals must be equipped with specialized knowledge and tools” and “advocate[s] for increased training.” Therefore, a measurable indicator would be the percentage of healthcare providers treating HIV patients who have received specialized training in managing concurrent mental health and substance use disorders, which would reflect the system’s capacity to provide holistic care.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being |
|
|
| SDG 10: Reduced Inequalities |
|
|
Source: bioengineer.org
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0