Some people with Arizona Medicaid are running into ‘ghost networks’ for mental health care – KJZZ

Report on Inaccurate Mental Health Provider Networks and Implications for Sustainable Development Goals
Introduction: The Challenge of “Ghost Networks” and SDG 3
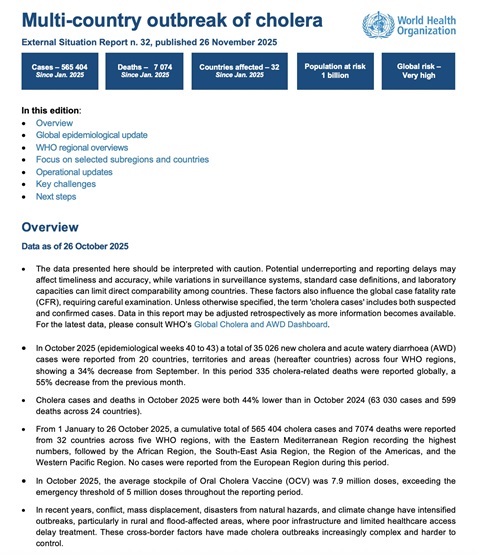
A significant barrier to mental healthcare access has been identified in the form of “ghost networks,” where health insurance provider directories are inflated with inactive or unavailable practitioners. This systemic failure directly contravenes the principles of Sustainable Development Goal 3 (Good Health and Well-being), which aims to ensure healthy lives and promote well-being for all at all ages. The inability of patients, such as the DeMarco family who waited nearly a decade for competent care, to find timely mental health services leads to worsening symptoms and repeated crises, undermining Target 3.4 concerning the promotion of mental health.
- “Ghost networks” are defined as provider directories that are largely unreachable, list out-of-network providers, or feature practitioners not accepting new patients.
- This issue affects both private Medicare Advantage and Medicaid managed care plans.
- The consequence for individuals with serious mental illness is a critical delay in care, exacerbating their conditions.
Federal Investigation Findings and Impact on SDG 10
A recent report from the Office of Inspector General (OIG) at the U.S. Department of Health and Human Services (HHS) quantifies the extent of these inaccuracies, revealing a failure that disproportionately affects vulnerable populations and widens health disparities. This situation presents a direct challenge to Sustainable Development Goal 10 (Reduced Inequalities) by creating unequal access to essential health services, particularly for those in rural and tribal communities who already face significant provider shortages.
- The HHS-OIG investigation reviewed plans across five states, including urban and rural counties in Arizona.
- The report found that a substantial percentage of listed behavioral health providers were inactive, having provided no services for an entire year.
- In the Medicare Advantage plans studied, 55% of listed behavioral health providers were found to be inactive.
- In Medicaid managed care plans, 28% of providers were inactive.
- These findings indicate that nearly three-quarters of the inactive providers should not have been listed in network directories, violating federal rules that mandate quarterly updates.
Systemic Barriers and their Relation to SDG 8 and SDG 16
The persistence of ghost networks is rooted in systemic issues that deter provider participation, impacting both the healthcare workforce and institutional accountability. These challenges relate to Sustainable Development Goal 8 (Decent Work and Economic Growth) by creating unsustainable working conditions for clinicians, and Sustainable Development Goal 16 (Peace, Justice and Strong Institutions) by highlighting a lack of effective and transparent institutional oversight in the administration of public health funds.
- Administrative Burden: Many providers cited overwhelming administrative requirements as a primary reason for ceasing participation in networks, describing a system where they feel like “cogs in a wheel versus clinicians.”
- Financial Unsustainability: Reimbursement rates that do not cover the actual cost of care make continued participation financially unviable for many practitioners.
- Institutional Failure: The problem reflects a breakdown in regulatory enforcement, as private insurers contracting with public programs like Medicaid fail to maintain the accurate provider networks required by federal law.
Recommendations and Institutional Responses
To address these systemic failures and align practices with SDG targets, the HHS-OIG has proposed concrete solutions aimed at improving transparency and reducing provider burdens. In response, state agencies like Arizona’s Health Care Cost Containment System (AHCCCS) have acknowledged the challenges and outlined corrective measures.
- HHS-OIG Recommendation 1: Reduce the administrative requirements placed upon providers to encourage network participation.
- HHS-OIG Recommendation 2: Create a centralized, nationwide provider directory to serve as a single, accurate source of information for all insurance plans.
- AHCCCS Response: The agency acknowledged the critical need for timely access and committed to improving transparency and accountability.
- AHCCCS Actions: Ongoing efforts include increased monitoring of network adequacy, reducing administrative hurdles, investing in the behavioral health workforce, and improving public-facing provider search tools.
Conclusion: A Call for Action to Uphold Health and Equality Goals
The prevalence of ghost networks represents a critical human crisis and a failure to implement existing policies designed to protect public health. The experience of families struggling to navigate these inaccurate systems underscores the urgent need for robust implementation and oversight. Fulfilling the commitments of the Sustainable Development Goals, particularly SDG 3, SDG 10, and SDG 16, requires moving beyond policy announcements to ensure that all individuals, regardless of location or income, have genuine access to the mental healthcare they need. The integrity of public health institutions and the well-being of the populace depend on rectifying this systemic issue.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
The article highlights issues directly related to several Sustainable Development Goals (SDGs). The primary connections are with health, inequality, and institutional effectiveness.
- SDG 3: Good Health and Well-being: The core theme of the article is the struggle to access mental health care, which is a fundamental component of overall health and well-being. The text describes how the lack of timely care for serious mental illness leads to “worsening symptoms, instability or repeated crises.”
- SDG 10: Reduced Inequalities: The article points to significant inequalities in healthcare access. It focuses on individuals enrolled in Medicaid, a program for people with limited income, and explicitly mentions that “rural and tribal communities remain the most impacted by provider shortages,” highlighting geographic and social disparities.
- SDG 16: Peace, Justice and Strong Institutions: The article examines the failures of institutions, including private insurance companies and government-managed care programs (AHCCCS). The existence of “ghost networks” demonstrates a lack of accountability and transparency, and the federal investigation by the Office of Inspector General (OIG) is an effort to enforce regulations and improve institutional effectiveness.
2. What specific targets under those SDGs can be identified based on the article’s content?
Based on the issues discussed, several specific SDG targets can be identified:
- Target 3.4: “By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.” The article’s focus on the difficulty of finding competent providers for severe mental health conditions directly relates to the “treatment” and “promotion of mental health and well-being” aspect of this target. The decade-long struggle of the DeMarco family to find care exemplifies the barriers to achieving this goal.
- Target 3.8: “Achieve universal health coverage, including financial risk protection, access to quality essential health-care services…” The article directly addresses the failure to provide “access to quality essential health-care services” for individuals covered by Medicaid and Medicare Advantage plans. The “ghost networks” are a clear barrier to the universal health coverage promised by these programs.
- Target 10.3: “Ensure equal opportunity and reduce inequalities of outcome…” The article highlights unequal outcomes in health access based on geographic location (urban vs. rural/tribal) and economic status (Medicaid recipients). The statement that “rural and tribal communities remain the most impacted” points directly to an inequality of outcome that this target aims to eliminate.
- Target 16.6: “Develop effective, accountable and transparent institutions at all levels.” The investigation into inaccurate provider directories by the HHS-OIG is a direct response to the lack of accountability and transparency from insurance companies. The article notes that these companies run counter to “federal rules requiring plans to keep their directories current,” indicating a failure of institutional effectiveness that this target seeks to address.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
Yes, the article mentions and implies several quantitative and qualitative indicators that can be used to measure progress.
- Percentage of inactive providers in network directories: This is a direct, quantifiable indicator mentioned in the article. The OIG report found that in the reviewed plans, “55% of listed behavioral health providers were inactive” in Medicare Advantage and “28% were inactive” in Medicaid managed care. Tracking this percentage over time would measure progress towards ensuring accurate directories and actual access to care (relevant to Targets 3.8 and 16.6).
- Provider-to-population ratio in different geographic areas: The article implies this indicator by stating that “rural and tribal communities remain the most impacted by provider shortages.” Measuring and comparing the number of active mental health providers per capita in urban, rural, and tribal areas would be a key indicator of health equity (relevant to Target 10.3).
- Wait times for accessing mental health services: The experience of the DeMarco family, who waited “nearly 10 years” to find a competent provider, implies that the time from seeking care to receiving it is a critical measure. Reducing this wait time is an indicator of improved access to mental health treatment (relevant to Target 3.4).
- Provider attrition rates from insurance networks: The article states that providers leave networks due to “overwhelming” administrative workloads and reimbursement rates that “do not cover the cost of care.” Tracking the rate at which providers leave these networks and the reasons why would serve as an indicator of the system’s sustainability and the effectiveness of institutional policies (relevant to Targets 3.8 and 16.6).
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being |
3.4: Promote mental health and well-being.
3.8: Achieve universal health coverage and access to quality essential health-care services. |
– Wait times for accessing competent mental health care. – Percentage of listed providers in insurance directories who are active and accepting new patients. |
| SDG 10: Reduced Inequalities | 10.3: Ensure equal opportunity and reduce inequalities of outcome. | – Disparity in the availability of mental health providers between urban, rural, and tribal communities. |
| SDG 16: Peace, Justice and Strong Institutions | 16.6: Develop effective, accountable and transparent institutions at all levels. |
– Compliance rate of insurance plans with federal regulations on updating provider directories. – Attrition rate of providers from insurance networks due to administrative burden or low reimbursement. |
Source: kjzz.org
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0