Sex-based differences in mortality among a large cohort of hospitalized patients with RT-PCR-confirmed SARS-CoV-2 infection at five different pandemic waves in Northern Iran – Nature
Report on Sex-Based Mortality Disparities in COVID-19 Patients
A Study Aligning with Sustainable Development Goals
Executive Summary
This report details a retrospective cohort study analyzing sex-based mortality disparities among 44,544 hospitalized, RT-PCR-confirmed COVID-19 patients in Northern Iran from 2019 to 2021. The analysis, crucial for advancing Sustainable Development Goal 3 (Good Health and Well-being) and SDG 5 (Gender Equality), reveals significant trends in pandemic-related mortality. After adjusting for confounders, males exhibited a 17% higher overall risk of death compared to females (OR: 1.17). Key determinants of mortality included age and the number of pre-existing health conditions, which showed a dose-responsive relationship with the odds of death. While overall mortality was higher in males, analysis of individual pandemic waves did not show a statistically significant difference in mortality odds between sexes for any single wave. These findings underscore the importance of disaggregated data in understanding health inequalities (SDG 10) and tailoring public health interventions to protect vulnerable populations.
1.0 Introduction: The COVID-19 Pandemic and the Sustainable Development Goals
The SARS-CoV-2 pandemic represents a significant setback to global progress on the Sustainable Development Goals (SDGs), particularly those related to health and equality. This study examines mortality determinants through the lens of these global goals.
1.1 A Global Health Crisis and SDG 3
The COVID-19 pandemic, with over 7 million deaths globally, has severely tested global health systems, directly impacting the targets of SDG 3 (Good Health and Well-being). Understanding the complex factors driving mortality, including viral variants, demographics, and comorbidities, is essential for building resilient healthcare systems and ensuring healthy lives for all.
1.2 Investigating Disparities: A Focus on SDG 5 and SDG 10
Initial evidence from the pandemic highlighted significant inequalities in health outcomes. This report focuses on two critical dimensions of inequality:
- SDG 5 (Gender Equality): Emerging data consistently showed higher mortality rates in men than women. This study investigates these sex-based differences to understand the biological and other factors that contribute to gender-specific health vulnerabilities.
- SDG 10 (Reduced Inequalities): Mortality risk is not evenly distributed. Factors such as age and pre-existing non-communicable diseases (NCDs) create highly vulnerable subgroups. This analysis aims to identify these groups to inform targeted public health strategies that reduce health inequalities.
1.3 Study Objectives
To address these gaps and contribute to the SDG framework, this study aimed to analyze sex-specific mortality trends and associated risk factors across five distinct pandemic waves among RT-PCR-confirmed hospitalized patients in Iran.
2.0 Methodology
The study employed a robust methodological framework to ensure the reliability of findings, adhering to the STROBE guidelines for observational studies.
2.1 Study Design and Population
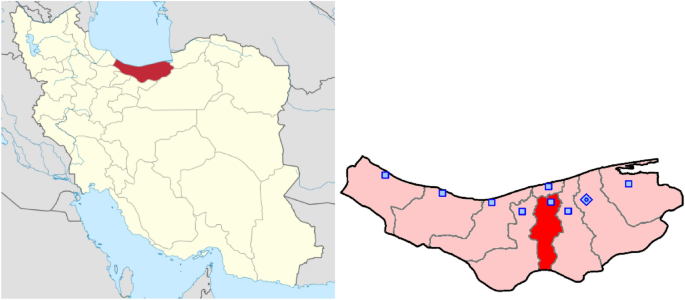
A retrospective cohort study was conducted using data from the Mazandaran Medical Care Monitoring Center (MCMC) registry. The final cohort included 44,544 hospitalized patients with RT-PCR-confirmed SARS-CoV-2 infection between 2019 and 2021. This comprehensive data registry exemplifies the type of integrated system needed to achieve SDG 17 (Partnerships for the Goals) by facilitating evidence-based health system analysis.
2.2 Variables and Data Collection
Data were collected on the following variables:
- Demographics: Age and sex.
- Comorbidities: Diabetes, hypertension, cancer, cardiac diseases, CKD, COPD, and chronic neurologic disorders.
- Clinical Data: Oxygen saturation (SpO2), need for intubation, and final outcome (cured or in-hospital mortality).
- Pandemic Wave: Patients were categorized into one of five pandemic peaks.
2.3 Pandemic Wave Classification
The five pandemic peaks were defined based on established epidemiological periods in Iran:
- First Peak: March 7, 2020 – May 16, 2020
- Second Peak: June 10, 2020 – September 5, 2020
- Third Peak: November 25, 2020 – March 5, 2021
- Fourth Peak: March 25, 2021 – May 31, 2021
- Fifth Peak: June 26, 2021 – December 1, 2021
2.4 Statistical Analysis
Multiple logistic regression models were used to calculate the odds ratio (OR) of COVID-19-related death, adjusting for potential confounders. Analyses were conducted for the total population and stratified by sex to identify specific risk profiles, thereby providing disaggregated data crucial for achieving SDG 5 and SDG 10.
3.0 Results: Quantifying Health Inequalities
The analysis of 44,544 patients (20,332 males, 24,212 females) yielded key insights into mortality patterns and their alignment with health-related SDGs.
3.1 Overall Mortality Disparities (SDG 3 & SDG 5)
A significant sex-based disparity in mortality was confirmed. After adjusting for age and comorbidities, males had a 17% higher odds of death compared to females (OR: 1.17, 95% CI: 1.09–1.25). This finding highlights a critical gender-specific vulnerability that public health strategies must address to achieve the goals of SDG 5.
3.2 The Impact of Age and Comorbidities (SDG 3 & SDG 10)
The study identified age and multimorbidity as primary drivers of mortality, exposing profound health inequalities affecting vulnerable populations.
- Age: A clear dose-responsive relationship was observed, with the odds of death increasing significantly with each age decade. Compared to patients under 20, those aged 80 and above had an 18-fold higher odds of death in the unadjusted model.
- Comorbidities: The number of comorbidities was strongly associated with mortality. Compared to patients with no comorbidities, the adjusted odds of death were:
- 1.23 times higher for one comorbidity.
- 1.47 times higher for two comorbidities.
- 1.75 times higher for three or more comorbidities.
These results underscore the challenge NCDs pose to achieving SDG 3 and the need for policies that reduce inequalities for older adults and those with chronic conditions (SDG 10).
3.3 Wave-Specific Mortality Trends
Mortality risk varied across pandemic waves, with the highest odds of death observed in the first and second peaks compared to the fifth. When stratified by sex and wave, the analysis revealed nuanced patterns. For instance, in the second peak, females had a slightly higher odds of death than males (OR 1.34 vs. 1.20), though the difference was not statistically significant. Overall, no significant sex-based difference in mortality was found within any individual peak, suggesting that while an overall disparity exists, its manifestation may be influenced by factors like dominant viral variants and evolving treatment protocols.
4.0 Discussion: Implications for Health Equity and Policy
4.1 Sex-Based Disparities and SDG 5
The finding of a 17% higher overall mortality risk for males aligns with global data and reinforces the need to integrate a gender perspective into health research and emergency response, a core tenet of SDG 5. The underlying biological mechanisms—including differences in immune response, hormonal profiles, and ACE2 receptor expression—point to the necessity of sex-disaggregated research to develop effective and equitable clinical interventions.
4.2 Temporal Variations and Health System Resilience (SDG 3)
The decline in mortality odds in later waves, despite the emergence of more transmissible variants like Delta, may reflect improved clinical management and health system adaptation over time. This highlights the importance of continuous learning and capacity building within healthcare systems to uphold the objectives of SDG 3 during prolonged health crises.
4.3 The Critical Role of Age and Comorbidities (SDG 3 & SDG 10)
The dose-responsive effect of age and multimorbidity on mortality risk is a stark reminder of the vulnerability of specific population segments. Protecting these groups is fundamental to reducing health inequalities (SDG 10) and ensuring that no one is left behind. Public health policies must prioritize these individuals for vaccination, early treatment, and ongoing management of NCDs to build resilience against future health threats.
5.0 Limitations and Policy Implications
5.1 Study Limitations
This report acknowledges certain limitations, including the exclusion of out-of-hospital deaths and the lack of data on vaccination status, specific treatments, and socioeconomic determinants. These factors are known to contribute to health inequalities and should be considered in future research.
5.2 Policy Implications for Sustainable Development
The findings support the following policy recommendations to advance the SDGs:
- Strengthen Health Monitoring (SDG 3): Prioritize early and aggressive monitoring for high-risk patients, particularly older adults and those with multiple comorbidities, irrespective of sex.
- Promote Gender-Responsive Health (SDG 5): Maintain heightened clinical vigilance for male patients, who face a higher overall mortality risk, and continue research into the biological and social drivers of this disparity.
- Reduce Health Inequalities (SDG 10): Target public health interventions, including vaccination and booster campaigns, toward older adults and individuals with NCDs to mitigate their heightened risk.
6.0 Conclusion
This study provides critical, data-driven insights into the sex-based and comorbidity-related disparities in COVID-19 mortality. The findings confirm that males, older adults, and individuals with multiple comorbidities face a disproportionately high risk of death. By quantifying these inequalities, this research contributes valuable evidence for shaping public health policies that are not only effective but also equitable, thereby supporting the global commitment to achieve Sustainable Development Goal 3 (Good Health and Well-being), SDG 5 (Gender Equality), and SDG 10 (Reduced Inequalities).
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
- The article’s primary focus is on understanding the mortality burden of the COVID-19 pandemic, a major global health crisis. It investigates factors influencing death rates, such as comorbidities (diabetes, cancer, cardiac diseases), which directly relates to ensuring healthy lives and promoting well-being for all at all ages. The study analyzes data from hospitalized patients to inform public health interventions and clinical management, contributing to the overall goal of improving health outcomes.
-
SDG 5: Gender Equality
- A central theme of the article is the analysis of “significant sex-based disparities in mortality,” with a specific focus on why men experienced higher death rates. By investigating and quantifying these differences (e.g., “Males were at 17% higher risk of death compared to women”), the study addresses the need to understand and tackle inequalities in health outcomes between sexes, which is a crucial aspect of gender equality.
-
SDG 10: Reduced Inequalities
- The research highlights inequalities in health outcomes based on factors other than sex. The article explicitly states that a “dose-responsive relationship between age, number of comorbidities, and death was observed.” This finding underscores how vulnerability to severe disease and death is not equally distributed across the population but is significantly higher for older individuals and those with pre-existing health conditions, aligning with the goal of reducing inequalities within and among countries.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
SDG 3: Good Health and Well-being
- Target 3.3: “By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.” The article directly contributes to this target by analyzing mortality determinants of COVID-19, a major communicable disease pandemic, to “inform effective public health interventions and clinical management strategies.”
- Target 3.4: “By 2030, reduce by one third premature mortality from non-communicable diseases…” The study finds that comorbidities such as “diabetes, cancer, cardiac diseases, chronic neurological diseases, and COPD were significantly associated with death.” This highlights the critical link between non-communicable diseases (NCDs) and mortality from communicable diseases, making the management of NCDs essential for overall health resilience.
- Target 3.d: “Strengthen the capacity of all countries… for early warning, risk reduction and management of national and global health risks.” The study utilizes the “Mazandaran Medical Care Monitoring Center (MCMC) data registry,” a comprehensive system that aggregates real-time health data. This represents a strengthened national capacity for health surveillance and research, which is crucial for managing health crises like the COVID-19 pandemic.
-
SDG 5: Gender Equality
- Target 5.1: “End all forms of discrimination against all women and girls everywhere.” While the study finds higher mortality in men, its detailed analysis of sex-based disparities in health is fundamental to achieving equality. Understanding these differences is the first step toward creating health policies and clinical guidelines that provide equitable care and outcomes for all sexes.
-
SDG 10: Reduced Inequalities
- Target 10.2: “By 2030, empower and promote the social, economic and political inclusion of all, irrespective of age, sex, disability, race, ethnicity, origin, religion or economic or other status.” The article’s conclusion that “age and the number of comorbidities demonstrated a significant association with mortality” directly addresses health outcome inequalities based on age and health status (a form of disability).
- Target 10.3: “Ensure equal opportunity and reduce inequalities of outcome…” The study’s “Policy and clinical implications” section recommends prioritizing vulnerable groups, such as older men with comorbidities, for monitoring and vaccination. This is a direct attempt to formulate policies that reduce inequalities of outcome (i.e., death) by providing targeted care.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Indicators for SDG 3
- Mortality rate due to COVID-19: The entire study is centered on measuring and analyzing COVID-19 related deaths. The article provides specific mortality proportions: “A higher proportion of males (9.8%) suffered mortality compared to females (7.9%).” This serves as a direct indicator for Target 3.3.
- Increased risk of mortality associated with non-communicable diseases: The article quantifies the impact of NCDs on COVID-19 mortality using Odds Ratios (OR). For example, it states that comorbidities like “DM (OR: 1.91), HTN (OR: 1.97), cancer (OR: 2.47), heart diseases (OR: 2.31), CKD (OR: 3.60)…” lead to higher odds of death. This serves as a powerful indicator for Target 3.4, measuring the mortality burden from the interaction of communicable and non-communicable diseases.
- Existence of a comprehensive health data registry: The article describes the “MCMC data registry” as a “significant resource for health services research due to its comprehensive, integrated, and operationally focused data ecosystem.” The establishment and use of such a registry is an implied indicator of a country’s strengthened capacity for health surveillance under Target 3.d.
-
Indicators for SDG 5
- Sex-disaggregated mortality data: The study is built upon collecting and analyzing mortality data broken down by sex. The core finding that “males were at 17% higher odds of death compared to women (OR: 1.17…)” is a key quantitative indicator used to measure health disparities between sexes, relevant to Target 5.1.
-
Indicators for SDG 10
- Mortality rate stratified by age group: The article provides clear evidence of age-based inequality, stating that “older age groups were significantly associated with higher odds of death, with dose-responsive behavior” and provides specific Odds Ratios for different age brackets (e.g., “OR: 18.06 in ≥ 80 years old patients”). This is a direct indicator for measuring inequality of outcome under Targets 10.2 and 10.3.
- Mortality risk stratified by number of comorbidities: The study shows that “the number of comorbidities also presented a significant dose-responsive increase in the odds of death.” It quantifies this by stating that patients with one, two, or at least three comorbidities had “1.87, 2.78, and 3.59 fold higher odds of death, respectively.” This measures inequality based on health status.
4. Summary Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators Identified in the Article |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.3: Combat communicable diseases.
3.4: Reduce premature mortality from non-communicable diseases. 3.d: Strengthen capacity for management of national and global health risks. |
– Mortality rate due to COVID-19.
– Odds Ratio (OR) of death for patients with specific non-communicable diseases (e.g., diabetes, cancer, cardiac diseases). – Existence and utilization of a comprehensive, real-time health data registry (MCMC). |
| SDG 5: Gender Equality | 5.1: End all forms of discrimination and ensure equality in outcomes. | – Sex-disaggregated mortality rates (9.8% for males vs. 7.9% for females). – Odds Ratio (OR) of death for males compared to females (OR: 1.17). |
| SDG 10: Reduced Inequalities | 10.2: Promote inclusion of all, irrespective of age or disability/health status.
10.3: Ensure equal opportunity and reduce inequalities of outcome. |
– Mortality rate and Odds Ratio of death stratified by age group.
– Odds Ratio of death stratified by the number of comorbidities (demonstrating a dose-responsive increase in risk). |
Source: nature.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0