Trajectory subgroups and influencing factors of nutrition-related risk in older NSCLC patients undergoing chemotherapy – BMC Geriatrics
Report on Nutritional Risk Trajectories in Older Cancer Patients and Alignment with Sustainable Development Goals
Introduction: Advancing SDG 3 Through Targeted Nutritional Care
A novel study utilizing Latent Class Growth Modeling (LCGM) has explored the trajectories of nutrition-related risk over six chemotherapy cycles in older adults with advanced Non-Small Cell Lung Cancer (NSCLC). This research provides a critical foundation for developing individualized interventions that align with Sustainable Development Goal 3 (SDG 3), which aims to ensure healthy lives and promote well-being for all at all ages. By focusing on a vulnerable population, the study directly contributes to the goal of reducing premature mortality from non-communicable diseases through effective treatment and care.
Identification of Heterogeneous Nutritional Risk Trajectories
The longitudinal analysis identified three distinct subgroups, revealing significant heterogeneity in how older patients respond to the nutritional challenges of chemotherapy. This differentiation is vital for moving beyond one-size-fits-all approaches and developing targeted strategies essential for achieving universal health coverage as envisioned in SDG 3.
- Group 1: Stable Low Risk (53.3%): Represents a majority of patients with robust nutritional reserves capable of withstanding treatment-induced stress.
- Group 2: Improving Moderate Risk (35.1%): A significant portion of patients who are initially vulnerable but show capacity for improvement, likely due to effective supportive care.
- Group 3: Persistent High to Moderate Risk (11.6%): A clinically critical subgroup that remains at elevated nutritional risk throughout treatment, facing a higher likelihood of complications and adverse outcomes.
Predictors of Vulnerability: Addressing SDG 10 (Reduced Inequalities)
The study identified key predictors that place patients in the most vulnerable trajectory group, highlighting a clear health inequality that must be addressed to fulfill the mandate of SDG 10 (Reduced Inequalities). By pinpointing these factors, healthcare systems can proactively identify and support those at greatest risk, ensuring no one is left behind.
Key Predictors for High-Risk Trajectory:
- Older Age: Associated with diminished metabolic reserves, sarcopenia, and reduced resilience to physiological stressors.
- Smoking History: Contributes to systemic inflammation, suppressed appetite, and altered taste perception, compounding nutritional challenges.
- Hypertension: May act as a marker for underlying conditions like endothelial dysfunction and chronic low-grade inflammation, which are linked to cancer cachexia and can be exacerbated by certain medications.
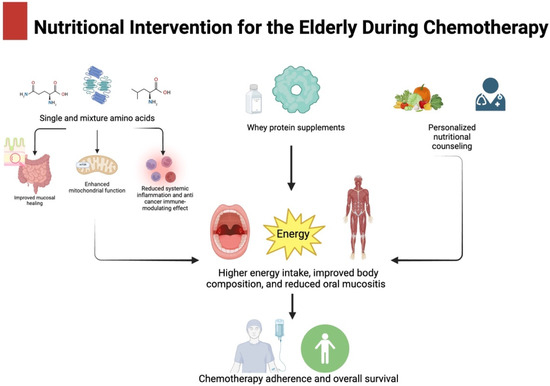
A Framework for Action: Integrating SDG 2 and SDG 3
The findings support a proactive, evidence-based management framework that directly contributes to SDG 2 (Zero Hunger), particularly Target 2.2 to end all forms of malnutrition, and SDG 3. By stratifying patients at the initiation of treatment, resources can be allocated efficiently to improve health outcomes, enhance quality of life, and reduce treatment-related toxicity.
- Persistent High to Moderate Risk Group: This group requires immediate and intensive intervention to mitigate the risks of malnutrition. This includes individualized dietary counseling, proactive symptom management, early use of nutritional supplements, and a multidisciplinary care approach involving oncologists, dietitians, and palliative care specialists. This targeted support is crucial for improving health equity (SDG 10).
- Improving Moderate Risk Group: This cohort warrants close monitoring and proactive support to sustain their positive trajectory. Regular screening and prompt intervention for emerging nutritional issues are key to ensuring their continued well-being (SDG 3).
- Stable Low Risk Group: This group benefits from routine monitoring and general nutritional education to prevent any unexpected deterioration and maintain their robust health status.
Study Considerations and Path Forward for Global Health Goals
The study possesses significant strengths, including its advanced longitudinal modeling and focus on an understudied, vulnerable population. However, certain limitations must be acknowledged to guide future research aimed at achieving global health goals.
Limitations:
- The observational and single-center design limits generalizability and precludes causal inference.
- The requirement for complete data across all six cycles may have selected for a more treatment-tolerant patient population.
- Unmeasured factors, such as specific dietary intake or inflammatory biomarkers, could represent residual confounders.
Future prospective, multi-center studies are warranted to validate these findings. Such research is essential for developing scalable clinical screening tools that can be implemented globally to identify high-risk patients, thereby advancing progress on SDG 3 and SDG 10 by ensuring equitable and effective nutritional care for all older adults with cancer.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
SDG 2: Zero Hunger
- The article’s primary focus is on “nutrition-related risk,” “nutritional status,” and “malnutrition complications” in a vulnerable population. This directly aligns with SDG 2, which aims to end hunger, achieve food security, and improve nutrition for all. The study investigates how to optimize nutrition for older adults with cancer, a key demographic mentioned in the goal’s targets.
SDG 3: Good Health and Well-being
- The article is fundamentally a health study centered on patients with non-small cell lung cancer (NSCLC), a non-communicable disease (NCD). It explores factors like age, smoking, and hypertension that affect health outcomes during chemotherapy. By aiming to improve treatment tolerance, reduce complications, and enhance “survival outcomes,” the research directly contributes to the objectives of SDG 3, which include reducing mortality from NCDs and ensuring healthy lives.
2. What specific targets under those SDGs can be identified based on the article’s content?
SDG 2: Zero Hunger
- Target 2.2: “By 2030, end all forms of malnutrition… and address the nutritional needs of… older persons.”
- The article is explicitly focused on this target. It studies “trajectories of nutrition-related risk” specifically in “older adults” and identifies a “persistent high to moderate risk group (Group 3, 11.6%)” that is at significant risk for malnutrition. The proposed “evidence-based management framework” is a direct strategy to “address the nutritional needs” of this vulnerable group.
SDG 3: Good Health and Well-being
- Target 3.4: “By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment…”
- The article addresses the treatment of NSCLC, a major non-communicable disease. It notes that unmanaged nutritional risk can lead to “increased treatment toxicity, dose reductions or delays… and potentially worse survival outcomes.” By identifying high-risk patients and proposing “early and aggressive nutritional support,” the study aims to improve treatment effectiveness and, consequently, reduce mortality from this NCD.
- Target 3.8: “Achieve universal health coverage, including… access to quality essential health-care services…”
- The study suggests that favorable outcomes may be “primarily attributable to the standardized supportive care and nutritional management implemented at our tertiary care center.” It also recommends a multidisciplinary team approach involving “oncologists, dietitians, nurses, pharmacists, and potentially geriatricians or palliative care specialists.” This highlights the importance of integrated, quality healthcare services, a core component of universal health coverage.
- Target 3.a: “Strengthen the implementation of the World Health Organization Framework Convention on Tobacco Control…”
- The research identifies “smoking history” as a key predictor for the “adverse high to moderate risk trajectory.” This finding underscores the detrimental impact of tobacco use on health outcomes, even during cancer treatment, thereby reinforcing the importance of tobacco control measures as a public health priority.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
Indicators for SDG 2 Targets
- Implied Indicator for Target 2.2: Prevalence of malnutrition/nutritional risk in specific populations.
- The article doesn’t use the official SDG indicator terminology but provides a direct measurement of nutritional risk. The classification of patients into three trajectory subgroups (“stable low risk group (53.3%)”, “improving moderate risk group (35.1%)”, and “persistent high to moderate risk group (11.6%)”) serves as a proxy indicator for the prevalence and severity of nutritional risk within the studied population of older adults with NSCLC.
Indicators for SDG 3 Targets
- Implied Indicator for Target 3.4: Mortality rate attributed to cancer, cardiovascular disease, diabetes or chronic respiratory disease (NCDs).
- The article links poor nutritional status in the high-risk group to “potentially worse survival outcomes.” Therefore, patient survival rates and mortality rates are the ultimate, albeit implied, indicators for measuring the success of the proposed nutritional interventions in improving treatment outcomes for this NCD.
- Implied Indicator for Target 3.8: Proportion of the population with access to essential health services.
- The article’s reference to “standardized supportive care and nutritional management” and the proposed “multidisciplinary team” approach implies that the availability and integration of such specialized services are key to patient care. The extent to which these services are available and utilized can serve as an indicator of access to quality, essential healthcare.
- Implied Indicator for Target 3.a: Prevalence of current tobacco use.
- The study’s identification of “smoking history” as a significant predictor of poor outcomes directly links tobacco use to adverse health events. This reinforces the relevance of tracking the prevalence of smoking as a key public health indicator to measure progress in tobacco control.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators Identified in the Article (Implied or Direct) |
|---|---|---|
| SDG 2: Zero Hunger | 2.2: End all forms of malnutrition, particularly for older persons. | Prevalence of nutritional risk, measured by the percentage of patients in different risk trajectories (e.g., “11.6%” in the persistent high-risk group). |
| SDG 3: Good Health and Well-being | 3.4: Reduce premature mortality from non-communicable diseases (NCDs) through treatment. | Patient survival rates and mortality rates from NSCLC, as the article links nutritional status to “potentially worse survival outcomes.” |
| 3.8: Achieve universal health coverage and access to quality essential health-care services. | Availability and integration of “standardized supportive care and nutritional management” and “multidisciplinary” teams within healthcare settings. | |
| 3.a: Strengthen the implementation of the WHO Framework Convention on Tobacco Control. | Prevalence of “smoking history” as a key risk factor, highlighting the importance of tracking tobacco use. |
Source: bmcgeriatr.biomedcentral.com
What is Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0



















































;Resize=620#)






















